Ovarian Cancer
Ovarian cancer starts in the cells of the ovary. A cancerous (malignant) tumor is a collection of cells that can invade and destroy the tissues around it. It can also spread (metastasize) to other parts of the body. Ovarian cancer tumors are classified according to the type of cells in which the cancer occurs.
Epithelial carcinoma of the ovary starts in the epithelial cells. It is the most common type of ovarian cancer. Serous carcinoma is the most common type of epithelial carcinoma of the ovary.
It is now believed that many serous ovarian carcinomas have originated from cells in the nearby fallopian tube that have attached to the surface of the affected ovary.
Tumors bordering on malignancy also appear in epithelial cells. When viewed under a microscope, they have some characteristics of carcinoma, but not all. They usually do not spread to nearby tissues or other parts of the body. Tumors bordering on malignancy include serous tumors and mucinous tumors.
Stromal tumors start in stromal cells. Of the stromal tumors that may be malignant, granulosa tumors are the most common type.
Germ cell tumors appear in germ cells. Of all ovarian tumors, mature cystic teratoma (dermoid cyst) is the most common type. Usually it is not cancerous. The most common type of cancerous germ cell tumor is dysgerminoma.
Primary serous peritoneal carcinoma can develop in the peritoneum, the membrane that lines the walls of the abdomen and pelvis. It is similar to epithelial ovarian cancer, but very little or no cancer is found in the ovary and it is not known for sure where the cancer started.
The changes that can occur in the cells of the ovary do not always lead to cancer. They can cause non-cancerous conditions like cysts or non-cancerous tumors like fibibroma.
Ovaries
The ovaries are the organs of the female reproductive system that produce eggs. There are two, buried deep in the woman’s pelvis, on either side of the uterus, near the end of the fallopian tubes.
Function
The ovaries have two main functions. They synthesize female sex hormones and produce mature eggs.
The female sex hormones are estrogen and progesterone. The ovaries are the most important source.
Estrogen is the main female sex hormone. This is responsible for the growth of the breasts and reproductive organs of women as well as the shape of their bodies.
Progesterone prepares the body for conception by causing the lining of the uterus (called the endometrium) to thicken. It also regulates menstruation and pregnancy.
Each month during ovulation, an ovary releases a mature egg. This then takes a fallopian tube to get to the uterus. If the egg is fertilized by a sperm, it attaches to the lining of the uterus (implantation) and begins to develop to form a fetus. If it is not fertilized, it is expelled from the body along with the lining of the uterus (menstruation).
At menopause, the ovaries stop releasing eggs and making sex hormones.
Types of ovarian cancer
Here’s a brief explanation of the types of ovarian cancers:
Epithelial ovarian cancer:
- This is the most common type of ovarian cancer, accounting for about 90% of all cases.
- It starts in the cells that cover the surface of the ovaries.
- There are several different types of epithelial ovarian cancer, including:
- Serous carcinoma: This is the most common type of epithelial ovarian cancer, accounting for about 70% of all cases. It can be further classified as high-grade or low-grade, depending on how abnormal the cells look under a microscope.
- Endometrioid carcinoma: This type of cancer is similar to endometrial cancer, which is a cancer of the lining of the uterus. It accounts for about 10% of all cases of epithelial ovarian cancer.
- Mucinous carcinoma: This type of cancer forms mucus-filled cysts in the ovaries. It accounts for about 6% of all cases of epithelial ovarian cancer.
- Clear cell carcinoma: This is a rare type of epithelial ovarian cancer that accounts for about 10% of all cases. It is more aggressive than other types of epithelial ovarian cancer.
Germ cell tumors:
- These are less common than epithelial ovarian cancers, accounting for about 3% of all cases.
- They start in the cells that produce eggs.
- There are several different types of germ cell tumors, including:
- Dysgerminoma: This is the most common type of germ cell tumor, accounting for about 50% of all cases. It is usually found in young women.
- Teratoma: This type of tumor can contain hair, teeth, and other tissues. It is usually found in young women.
- Embryonal carcinoma: This is a more aggressive type of germ cell tumor that is often found in young children.
- Yolk sac tumor: This is a rare type of germ cell tumor that is usually found in young children.
Stromal tumors:
- These are the rarest type of ovarian cancer, accounting for about 1% of all cases.
- They start in the connective tissue of the ovaries.
- There are two main types of stromal tumors:
- Granulosa cell tumors: These are the most common type of stromal tumor. They are usually benign, but they can become cancerous.
- Sertoli-Leydig cell tumors: These are even rarer than granulosa cell tumors. They can be benign or malignant.
Borderline ovarian tumors:
- These are tumors that have some of the characteristics of cancer, but they are not considered to be cancerous.
- They are usually found in young women and have a very good prognosis.
Other types of ovarian cancer:
- Carcinosarcoma: This is a rare type of ovarian cancer that contains both epithelial and stromal cancer cells.
- Undifferentiated carcinoma: This is a type of ovarian cancer that does not look like any other type of ovarian cancer.
It is important to note that this is not an exhaustive list of all types of ovarian cancer. If you have any questions or concerns about your own health, please talk to your doctor.
Symptoms of ovarian cancer
Ovarian cancer may not cause any signs or symptoms in the very early stages of the disease. Signs and symptoms usually appear when the tumor grows and causes changes in the body. Other medical conditions can cause the same symptoms as ovarian cancer.
How do know if you have ovarian cancer? The signs and symptoms of ovarian cancer include the following:
- abnormal vaginal bleeding (for example, bleeding that is heavy, irregular, or occurs between periods), especially after menopause
- frequent discharge from the vagina that is clear, white or tinged with blood
- palpable mass in the pelvis or abdomen
- bladder problems, such as the need to urinate frequently and the urge to urinate
- constipation
- digestive changes, such as feeling full after a light meal, loss of appetite, heartburn, gas, difficulty digesting, or nausea
- frequent feeling of pressure in the pelvis or abdomen
- tired
- pain in the legs, lower back, pelvis or abdomen
- pain during sex
- swelling of the abdomen
- weightloss
- accumulation of fluid in the abdomen (ascites), around the lungs (pleural effusion) or in the legs (lymphedema)
difficulty in breathing
Risk of ovarian cancer
Certain behaviors, substances, or conditions can affect your risk, or likelihood, of getting cancer. There are things that increase your risk while others decrease it. Most cancers are caused by many risks. But cancer sometimes appears in people who are not at risk.
Epithelial ovarian carcinoma is the most common type of ovarian cancer. The number of new cases (incidence) of this cancer increases with age. Most epithelial carcinomas of the ovary are seen in women who have completed menopause.
Some people with particular genetic disorders have a higher than average risk of developing ovarian cancer. Discuss your risk with your doctor. If you have a genetic disorder that increases your risk for ovarian cancer, you may need to see your doctor more often to check for ovarian cancer. Your doctor will tell you which tests to take and how often.
The following may increase or reduce your risk for epithelial ovarian carcinoma. The risks of less common types of ovarian cancer are not well known and may differ from those of epithelial ovarian carcinoma. But many of the risk factors for epithelial ovarian carcinoma are the same as those for cancer of the fallopian tube. Some experts believe this may be because some epithelial ovarian carcinomas start in a fallopian tube.
- Family history of ovarian cancer
- BRCA gene mutations
- Lynch Syndrome
- Family history of certain cancers
- Personal history of breast cancer
- Pregnancy
- Gynecological surgery
- Hormone replacement therapy (HRT)
- Oral contraceptives
- Smoking tobacco
- Asbestos
- Tall adult height
- Excess weight
- Endometriosis
- Sedentary behavior
Family history of ovarian cancer
When there is a family history of ovarian cancer, it means that 1 or more blood relatives have or have had this form of cancer. Sometimes there are more cases of ovarian cancer in a family than you might expect. It may not be known for sure whether this family disposition is due to chance, to a way of life that family members share, to a genetic risk passed down from parents to their children, or to an association. of these factors.
If more than one of your relatives has ovarian cancer, your risk of having it may be higher. These relatives can be on the maternal side or the paternal side.
You may be at a higher risk for ovarian cancer if a first-degree relative (mother, sister or daughter) has already had it. Your risk is higher if your mother was diagnosed with ovarian cancer rather than your daughter. Your risk may be even greater if this relative was diagnosed before she is 50 or has gone through the menopause.
Having at least 2 first-degree relatives who have been diagnosed with ovarian cancer also increases your risk.
Your risk may be slightly higher if 1 first degree relative and 1 second degree relative (aunt, grandmother or niece) are diagnosed with ovarian cancer.
BRCA gene mutations
Breast cancer gene 1 (BRCA1) and breast cancer gene 2 (BRCA2) normally help control the growth of cancer cells. Mutations in these genes (which can be passed on to a child from the father or mother) increase the risk of breast cancer. These mutations also increase the risk of ovarian cancer. But not all women with BRCA1 or BRCA2 mutations will develop ovarian cancer.
Overall, a mutation in the BRCA1 gene increases the risk of ovarian cancer more than a mutation in the BRCA2 gene. Women with a BRCA1 mutation are more likely to get ovarian cancer before the age of 50. Women with a BRCA2 mutation are more likely to develop ovarian cancer after the age of 60. Ovarian cancer is usually diagnosed at a younger age in women who do not have a BRCA gene mutation.
Ovarian cancer is probably linked to an inherited mutation in the BRCA1 or BRCA2 gene if:
several family members have breast or ovarian cancer;
1 or more relatives had breast cancer before they were 50 years old;
a relative has breast cancer and ovarian cancer;
family members have cancer in both breasts (bilateral breast cancer);
a male relative has breast cancer;
the female is of Ashkenazi Jewish (Eastern European) descent.
Serous carcinoma, which is a type of epithelial carcinoma of the ovary, is more often linked to mutations in BRCA genes than other types of ovarian cancer. Ovarian cancer linked to a mutation in the BRCA genes also increases the risk of papillary serous carcinoma of the peritoneum, which is cancer of the lining of the abdominal cavity.
Women with ovarian cancer linked to a BRCA gene mutation are also at increased risk of breast cancer and other cancers. Discuss your risks with your doctor. Genetic risk assessment might be an option for some women.
Lynch Syndrome
Lynch syndrome is an inherited disorder that causes a large number of polyps to form on the lining of the colon and rectum, but in fewer quantities than in familial adenomatous polyposis (FAP).
There are 2 types of Lynch syndrome. Type A increases the risk of colorectal cancer, while type B increases the risk of several cancers, including colorectal cancer and other cancers of the digestive system, as well as ovarian and ovarian cancers. uterus in women. Due to its link to colorectal cancer, Lynch syndrome is also called hereditary nonpolyposis colorectal cancer, or HNPCC.
Family history of certain cancers
Women who have a family history of breast cancer have a higher risk of developing ovarian cancer. A family history of colorectal, uterine or pancreatic cancer also increases the risk of ovarian cancer.
Personal history of breast cancer
Women who have been diagnosed with breast cancer are more likely to develop ovarian cancer. A mutation in the BRCA genes could be the cause. Certain risk factors for breast cancer related to a woman’s menstrual history may also increase the likelihood that she will one day develop ovarian cancer. These risk factors include the onset of your first period early (under 11) or the onset of menopause at an older age (after 55).
Pregnancy
Women who have never been pregnant are more likely to get ovarian cancer than women who have been pregnant before. Researchers believe this lower risk is due to hormones present during pregnancy that have a protective effect. It is also possible that the higher risk of women who have never been pregnant may be related to factors that could make it difficult for them to become pregnant.
The risk of ovarian cancer is also higher in women who have never given birth to a child, even if they have been pregnant. Researchers are not sure whether this increased risk is related to the same factors that increase the risk of ovarian cancer in women who have never been pregnant.
Having been pregnant in the past lowers your risk of developing ovarian cancer. The more pregnancies you have had, the greater the protective effect. Pregnancy, however, does not appear to have a protective effect in women who have a significant family history of ovarian cancer or who have a BRCA gene mutation.
Gynecological surgery
Tubal ligation is surgery that cuts or blocks the fallopian tubes. Salpingectomy is surgery to remove the fallopian tubes. Both of these surgeries reduce a woman’s risk of developing ovarian cancer.
Hysterectomy is surgery to remove the uterus. It may also reduce the risk of ovarian cancer, but not as much as tubal ligation. Hysterectomy appears to reduce the risk when the fallopian tubes and ovaries are also removed (bilateral salpingo-oophorectomy).
Bilateral salpingo-oophorectomy may be offered to women with a BRCA1 or BRCA2 gene mutation who are at higher risk of ovarian cancer to reduce this risk.
Hormone replacement therapy (HRT)
Hormone replacement therapy (HRT) uses female sex hormones (estrogen, progesterone, or both) to manage menopausal symptoms such as hot flashes, vaginal dryness, and mood swings.
Research suggests that estrogen-only HRT and combined HRT (estrogen and progesterone) increase the risk of ovarian cancer. The longer you take estrogen, the greater your risk. Women who have had HRT for more than 5 years are more likely to develop ovarian cancer than women who have had it for less than 5 years. Current users of HRT are at greater risk of developing an ovarian cancer only women who have stopped taking HRT, no matter how long.
Discuss the benefits and risks of HRT with your doctor.
Oral contraceptives
Oral contraceptives (the pill) are intended to prevent pregnancy. They contain two hormones, estrogen and progesterone. Oral contraceptives lower your risk of ovarian cancer.
Smoking tobacco
Smoking tobacco increases your risk of mucinous carcinoma, a type of epithelial carcinoma of the ovary in women.
Tobacco in all its forms – cigarettes, cigars and pipes – increases your risk. The longer you smoke and the longer you smoke, the higher your risk. After you quit smoking, your risk of developing mucinous carcinoma decreases over time.
Asbestos
Asbestos is a group of different natural minerals. It has been used extensively in building materials and many industries. Asbestos increases the risk of ovarian cancer.
Large in adulthood
Women who are tall have a slightly higher risk of developing ovarian cancer. Researchers believe this increased risk could be attributable to developmental factors like growth hormones and puberty.
Excess weight
Being overweight and obese increases the risk of ovarian cancer.
Endometriosis
The endometrium is the lining of the uterus. Endometriosis is characterized by the development of the endometrium outside the uterus. It can develop on the ovaries, behind the uterus, on the small intestine, on the large intestine, or on the bladder. The risk of developing ovarian cancer is higher in women with endometriosis, especially if the ovaries are affected. Other studies show that the risk of certain types of ovarian cancer, including clear cell tumors and endometrioid tumors, may be higher in women with endometriosis.
Sedentary behavior
Sedentary behavior, or spending a lot of time sitting down, increases your risk for ovarian cancer.
Possible risks
The following have been linked to ovarian cancer in some way, but there is not enough evidence to say that they are risks. We need to do more research.
Number of periods in your lifetime, number of ovulations in your lifetime, onset of menstruation before the age of 12 (early menstruation or early menarche) or stopping of menstruation after the age of 55 (late menopause )
Talcum powder
Insufficient consumption of vegetables
The following have been linked to a lower risk of ovarian cancer, but more research is needed to confirm that they reduce this risk.
Feeding with milk
Aspirin
Diagnosis of ovarian cancer
Diagnosis is the process of determining the cause of a health problem. The diagnostic process for ovarian cancer usually begins with a visit to your family doctor. Your doctor will ask you about your symptoms and do a physical exam. Based on this information, your doctor may refer you to a specialist or order tests to check for ovarian cancer or other health problems.
The diagnostic process can seem long and overwhelming. It’s okay to worry, but try to remember that other medical conditions can cause symptoms similar to ovarian cancer. It is important that the healthcare team rule out any other possible cause of the condition before making a diagnosis of ovarian cancer.
The following tests are usually used to rule out or confirm a diagnosis of ovarian cancer. Many tests that can make a diagnosis of cancer are also used to determine the stage (extent of progression of the disease). Your doctor may also order other tests to assess your general health and help plan your treatment.
Health history and physical examination
A health history is a history of symptoms, risk factors, and all of the medical events and conditions a person has had in the past. Your doctor will ask you questions about your history of:
symptoms that may indicate the presence of ovarian cancer
breast cancer
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer, or HNPCC syndrome)
pregnancy
hormone replacement therapy
smoking
asbestos exposure
Your doctor may also ask you about your family history of:
ovarian cancer or breast cancer
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer, or HNPCC syndrome)
infertility
risk factors for ovarian cancer
other cancers, such as breast cancer, uterine cancer, or colorectal cancer
The physical exam allows the doctor to look for signs of ovarian cancer. During the physical examination, he might:
- do a pelvic exam and rectal exam to check the uterus, vagina, ovaries, fallopian tubes, bladder, and rectum for any unusual changes
- feel the abdomen to check for lumps or bloating or if organs such as the liver or spleen have increased in size.
Ultrasound
In an ultrasound, high-frequency sound waves are used to produce images of certain parts of the body. A pelvic or transvaginal ultrasound can be done to check for ovarian cancer. In a transvaginal ultrasound, the probe is placed in the vagina and the waves are directed to the ovaries instead of placing it on the surface of the abdomen. Ultrasound is used to:
- find a lump in the ovary and see if it’s a solid tumor or a fluid-filled cyst
- see the shape and size of the ovary and observe its contents
- assess abnormalities in other organs of the pelvis
- check for fluid accumulation in the abdomen
Determination of tumor markers
Tumor markers are substances found in the blood, tissues and fluids taken from the body. Tumor marker assays are usually done to assess response to cancer treatment and to monitor for recurrence. It can also help diagnose ovarian cancer.
In the case of ovarian cancer, the following tumor markers can be assayed.
The dosage of tumor antigen 125 (CA 125) may be higher in women with ovarian cancer, a benign condition or other cancer.
The dosage of carcinoembryonic antigen (CEA) may be higher in women with ovarian cancer or other minor conditions.
The dosage of human chorionic gonadotropin (HCG or ß-HCG) may be higher in young women with germ cell tumor of the ovary.
The alpha-fetoprotein (AFP) dosage may be higher in young women with germ cell tumor of the ovary.
Complete blood count (CBC)
The complete blood count (CBC) is used to assess the quantity and quality of white blood cells, red blood cells and platelets. A CHF is done to get information about your condition, to check for anemia caused by long-lasting vaginal bleeding, and to get baselines that can be used. Compare the results of next FSC made during and after treatment.
Blood biochemical analyzes
In blood chemistry tests, the level of certain chemicals in the blood is measured. These analyzes make it possible to evaluate the functioning of certain organs and to detect abnormalities.
Lacticodehydrogenase (LDH) levels can be measured in women with ovarian cancer. A high level may indicate the presence of a germ cell tumor of the ovary.
Some hormones, such as estrogen, testosterone and inhibin, may be higher than normal in women with ovarian stromal tumors.
Computed tomography (CT)
A computed tomography (CT) scan uses special x-ray machines to produce 3-dimensional and cross-sectional images of organs, tissues, bones and blood vessels. A computer assembles the photos into detailed images.
CT is used for:
assess the pelvis, abdomen and lymph nodes surrounding the ovaries
determine if the cancer has spread to other organs or tissues
guide the needle during a biopsy to an area where it is believed there may be metastasis
Magnetic resonance imaging (MRI)
Magnetic resonance imaging (MRI) uses powerful magnetic forces and radio waves to produce cross-sectional images of organs, tissues, bones and blood vessels. A computer assembles the photos into 3-dimensional images.
MRI is used for:
assess the pelvis, abdomen and lymph nodes surrounding the ovaries
determine if the cancer has spread to other organs or tissues
guide the needle during a biopsy to an area where it is believed there may be metastasis
Laparoscopy
During a laparoscopy, the doctor inserts a thin tube (called a laparoscope) into the abdominal cavity through a small incision (cut) he made in the abdomen. He can slide surgical instruments into the laparoscope to remove small pieces of tissue. Laparoscopy is used to:
check for abnormal masses and take tissue samples from the ovaries and other organs in the abdomen
remove small tumors or cysts
help confirm the stage of cancer
plan surgery or other treatments
Biopsy
During a biopsy, the doctor removes tissues or cells from the body for analysis in the laboratory. A pathologist then prepares a report that indicates the presence or absence of cancer cells in the sample.
In ovarian cancer, the biopsy is usually done during a surgery called a laparotomy. It is used to diagnose, stage and treat ovarian cancer, often in a single operation. The surgeon makes a large incision (cut) in the abdomen to examine all the organs in the abdominal cavity. During this procedure, the surgeon usually removes the entire tumor and also takes tissue samples from different parts of the pelvis and abdomen to see if the cancer has spread there. The samples are sent to a laboratory to determine the stage of the cancer. This is called surgical staging.
Paracentesis
Paracentesis is a procedure in which a needle or a hollow tube is inserted through the skin into the abdominal cavity. It is used to remove a buildup of fluid in the abdomen (ascites) that causes symptoms. The fluid is then examined to see if it contains cancer cells.
Pulmonary radiography
In an x-ray, small doses of radiation are used to produce an image of certain parts of the body on film. It is used to check for signs of a buildup of fluid around the lungs (pleural effusion) which could be caused by ovarian cancer that has spread to the lungs.
Colonoscopy
A colonoscopy may be done to check if the ovarian cancer has spread to the colon or to confirm that there is no colon cancer.
Positron Emission Tomography (PET scan)
A positron emission tomography (PET Scan) scan uses a radioactive material called a radiopharmaceutical to detect changes in the metabolic activity of body tissues. A computer analyzes the distribution patterns of the radioactivity and produces 3-dimensional and color images of the examined region.
A PET may be used to find ovarian cancer that has come back (has come back) or has spread to other organs or tissues.
Tumor Markers: What They Are and How They’re Used to Diagnose and Monitor Cancer
Histological classification of ovarian cancer (grading)
The grade describes how cancer cells look compared to normal cells and how quickly they grow. To determine the grade of ovarian cancer, the pathologist examines a sample of tissue taken from the tumor under a microscope.
The word differentiation is used to refer to how different cancer cells are.
Low-grade cancer cells are usually well differentiated. They almost look like normal cells. They tend to grow slowly and are less likely to spread.
High-grade cancer cells are usually poorly differentiated or undifferentiated. Their appearance is less normal, or more abnormal. They tend to grow faster and are more likely to spread than low-grade cancer cells.
A peculiarity of serous epithelial ovarian cancer is that the name of the two tumor subtypes mentions the grade, established according to their appearance and behavior:
low-grade serous carcinoma (CSBG)
high-grade serous carcinoma (CSHG)
By definition, some ovarian cancers are high grade, such as clear cell carcinoma. The grade of other types of ovarian cancer is classified from 1 to 3, for example in the case of endometrioid adenocarcinoma. The lower the number, the lower the grade of cancer.
Knowing the grade gives your healthcare team an idea of how quickly cancer can grow and how likely it is to spread. It helps him plan your treatment. The grade can also help the healthcare team determine the possible outcome of the disease (the prognosis) and predict how the cancer might respond to treatment.
Stages of ovarian cancer
Staging describes or categorizes cancer based on how much cancer is in the body and where it was initially diagnosed. This is often referred to as the extent of cancer. Information from tests is used to find out how big the tumor is, what parts of the organ have cancer, if the cancer has spread from where it started and where it has spread. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The most frequently used staging system for ovarian cancer is the FIGO classification. In ovarian cancer there are 4 stages. For stages 1 to 4, we often use the Roman numerals I, II, III and IV, but, in order to make the text clearer, we will use the Arabic numerals 1, 2, 3 and 4. In general, more the higher the stage number, the more the cancer has spread. Talk to your doctor if you have questions about staging.
The FIGO staging system is applicable to epithelial tumors and ovarian stromal tumors, including borderline malignancy tumors. It is also used to determine the stage of cancers that start in the peritoneum (called primary peritoneal carcinomas).
The stage of ovarian cancer is established by surgery to remove the ovaries and as much of the tissue to which the cancer has spread as possible. All removed tissue is tested for cancer cells. The stage is determined according to the results of the examinations. It can be seen that the stage of some women who were thought to have early stage cancer (stage 1) is higher after full surgical staging.
Find out more about cancer staging
Stage 1
The tumor is found only in one or both ovary.
In stage 1A, the tumor is found inside only one of the ovaries and nowhere else. The capsule surrounding the ovary is not ruptured (it is intact).
In stage 1B, tumors are found inside both ovaries, but nowhere else. The capsule that surrounds each of the ovaries is not ruptured.
In stage 1C, the tumor is in one or both ovaries and one of the following is true:
The capsule surrounding the ovary broke during surgery (surgical spill).
The capsule surrounding the ovary broke before surgery. Cancer cells are found on the surface of one or both ovaries.
Cancer cells are present in ascites or peritoneal lavage fluid (saline solution used to wash the peritoneal cavity and check for cancer cells at the time of surgery).
Stage 2
Cancer is present in only one ovary or both and has invaded nearby organs in the pelvis.
In stage 2A, the tumor has grown into the uterus, fallopian tubes, or both.
In stage 2AB, the tumor has invaded other organs in the lower pelvis, such as the rectum.
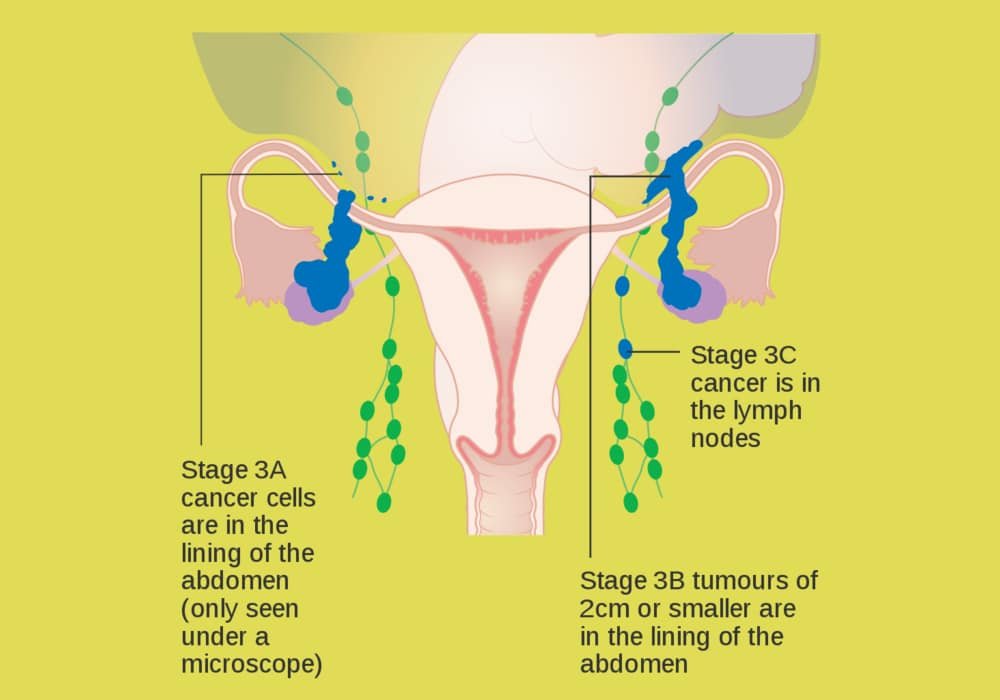
Stage 3
Cancer is present in only one or both ovaries where it started in the peritoneum. The cancer has spread to areas outside the pelvis.
In stage 3A, the cancer has spread to the lymph nodes in the back of the abdomen (retroperitoneal lymph nodes) or a small amount of cancer (seen only under a microscope) has spread to the peritoneum through outside the pelvis and into the intestine and it may have spread to the retroperitoneal lymph nodes.
In stage 3B, a large amount of cancer (seen by the doctor during surgery) has spread to the peritoneum just outside the pelvis and into the intestine and may have spread to the retroperitoneal lymph nodes.
In stage 3C, the cancer has spread to the peritoneum outside the pelvis and far from this structure (more than 2 cm away). It may be present on the capsule surrounding the liver or spleen, but it has not invaded the interior of these organs.
Stage 4
The cancer has spread to other parts of the body (distant metastases) located outside the abdomen and pelvis.
In stage 4A, cancer cells are seen in the fluid that has accumulated inside the pleural space (pleural effusion).
In stage 4B, the cancer has spread to other organs, such as the liver (inner part), lungs, or lymph nodes outside the abdomen.
Recurrence of ovarian cancer
If ovarian cancer comes back, the cancer comes back after treatment. If it reappears in the place where it first originated or near it, it is referred to as a local recurrence. It can also reappear in another part of the body: this is called a recurrence or distant metastasis.
If ovarian cancer spreads
Cancer cells can spread from the ovary to other parts of the body. This spread is called metastasis.
Understanding how a type of cancer tends to grow and spread helps your healthcare team plan for your treatment and future care. If ovarian cancer spreads, it can spread to the following structures:
- fallopian tube
- other ovary
- uterus
- cervix
- vagina
- omentum (fold of the peritoneum that covers and supports the organs and blood vessels in the abdomen)
parietal peritoneum (membrane that lines the walls of the abdomen and pelvis) or visceral peritoneum (membrane that covers and supports most of the abdominal organs)
diaphragm (thin muscle located under the lungs and heart that separates the chest cavity from the abdomen) - lymph nodes of the pelvis and retroperitoneum
- bladder
- large intestine
- rectum
- small intestine
- liver
- lungs
Prognosis and survival for ovarian cancer (Chances of Surviving)
If you have ovarian cancer, you may be wondering about your prognosis. Prognosis is the act by which a doctor best assesses how cancer will affect a person and how they will respond to treatment. The prognosis and survival depend on many factors. Only a doctor who is familiar with your medical history, the type, grade, stage and other characteristics of the cancer you have, the treatments chosen and the response to treatment can review all of this together with survival statistics. to arrive at a prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person affected (for example, whether or not they smoke) that the doctor takes into account when making a prognosis. A predictor factor influences how cancer responds to a certain treatment. We often discuss prognostic and predictive factors together. They both play a role in choosing the treatment plan and in establishing the prognosis.
The following are prognostic and predictive factors for ovarian cancer
Stadium
Stage is the most important prognostic factor for most types of ovarian cancer. A woman diagnosed with early stage ovarian cancer has a more favorable prognosis than a woman diagnosed with advanced ovarian cancer.
Presence of cancer cells in ascites fluid or peritoneal lavage
If ovarian cancer cells are present in ascites (a buildup of fluid in the abdomen) or in the peritoneal lavage fluid taken during surgery, the prognosis is poorer.
Extra-ovarian spread
Ovarian tumors can spread to other organs or other surfaces near the ovary. If there are a large number of tumors in the pelvis or abdomen, the prognosis is poorer.
Tumor type
Certain types of ovarian cancer have a better prognosis. The characteristics of a particular type of tumor are often related to the grade or stage of the tumor. For example, most ovarian stromal tumors are low grade and have a favorable prognosis.
Grade
The grade of a tumor is an important prognostic factor for ovarian cancer. Low-grade tumors have a more favorable prognosis than high-grade tumors.
Cancer remaining after surgery
Residual disease refers to the amount of cancer that remains after surgery. If there is no residual disease, the prognosis is more favorable than if there is cancer left after surgery.
Age
The prognosis of young women with ovarian cancer is more favorable than that of older women.
Functional index
The Functional Index measures how well a person is able to perform common tasks and daily activities. A woman with a good functional index is more likely to respond to treatment, experience fewer and more severe side effects, and have a more encouraging prognosis.
Reaction to chemotherapy
A reaction of the cancer to treatment after the first cycle of chemotherapy is considered a favorable prognostic factor.
Tumor antigen level 125 (CA 125)
A decrease in tumor antigen 125 (CA 125) levels after chemotherapy is a favorable prognostic factor.
Treatments for ovarian cancer
If you have ovarian cancer, your healthcare team will make a treatment plan especially for you. This plan will be based on your condition and cancer-specific information. When your healthcare team decides which treatments to offer you for ovarian cancer, they take the following into consideration:
- the stadium
- the rank
- the type of tumor
- if you want to bear children one day
You may be offered one or more of the following treatments for ovarian cancer
Surgery
Surgery is the main treatment for ovarian cancer, regardless of stage and type.
The most common operation is total hysterectomy with bilateral salpingo-oophorectomy. During surgery, the uterus, ovaries and fallopian tubes are removed. The surrounding lymph nodes, omentum, and any other tissues that appear abnormal at the time of surgery are sometimes also removed.
Salpingo-oophorectomy can be unilateral (i.e. removing the ovary and fallopian tube from one side only) or bilateral (i.e. removing both ovaries and both fallopian tubes).
In tumor reduction surgery, as much of the cancer in the abdomen as possible is removed.
In a cystectomy, only the cyst containing the tumor is removed and the rest of the ovary is left intact.
Some surgical procedures can be used to relieve the symptoms of advanced ovarian cancer.
Chemotherapy
Chemotherapy is offered before or after surgery to treat certain types and stages of ovarian cancer.
Chemotherapy can also be given to relieve pain or to control the symptoms of ovarian cancer (this is called palliative chemotherapy).
Hormone therapy
Some women with low-grade ovarian cancer may receive hormone therapy instead of chemotherapy after surgery.
Targeted treatment
Some women with epithelial ovarian cancer or advanced primary peritoneal carcinoma may receive targeted therapy, with or without chemotherapy.
Radiotherapy
Radiation therapy is not commonly used to treat ovarian cancer. Ovarian cancer often affects many organs in the abdomen, while radiation therapy should be directed to a small area. Radiation therapy can be used after surgery if a woman cannot receive chemotherapy because of her age or health problems. It can also be used to treat small areas where the cancer has come back (has come back) or has spread, or to control the symptoms of advanced ovarian cancer.
If you cannot or do not want to be treated for cancer
You may want to consider care that aims to make you feel better without treating the cancer itself, perhaps because cancer treatments no longer work, are no longer likely to improve your condition, or their side effects are difficult to tolerate. There may be other reasons why you cannot or do not want to be treated for cancer.
Talk to members of your healthcare team. They can help you choose advanced cancer care and treatment.
Monitoring
Follow-up after treatment is an important part of caring for people with cancer. You will need to have regular follow-up visits, especially during the first five years after the end of treatment. These visits will allow the healthcare team to monitor your progress and to know how you are recovering from treatment.
Clinical tests
A few clinical trials in ovarian cancer are underway in your country are accepting participants. Clinical trials aim to find new methods of preventing, detecting and treating cancer.
Supportive care for ovarian cancer
Supportive care empowers women to overcome the physical, practical, emotional and spiritual barriers of ovarian cancer. They are an important component of the care provided to people with this disease. There are many programs and services to meet the needs and improve the quality of life for them and their loved ones, especially after treatment is over.
Recovery from ovarian cancer and coping with life after treatment differs from woman to woman. They vary depending on the stage of the cancer, the organs and tissues removed by surgery, the type of treatment given and many other factors. The end of cancer treatment can lead to mixed emotions. Even if treatment is finished, there may be other issues to work out, such as coping with long-term side effects. A woman who has been treated for ovarian cancer may be concerned about the following.
Self-esteem and body image
Self-esteem refers to how a person feels about themselves. Body image refers to how a person perceives their own body. Ovarian cancer and its treatments can affect a woman’s self-esteem and body image, often because they lead to changes in the body, such as:
scars
hair loss
changes in body weight
sexual disturbances
Some of these changes may be temporary, while others will last a long time or be permanent.
For many women, body image and the way they see themselves in the eyes of others is closely linked to self-esteem. This may be a real concern that could cause considerable distress. These women may feel anger, worry or pain, be afraid to go out, or fear being rejected by others, although the effects of treatment may not be visible.
Lymphedema
Lymphedema is a form of swelling that occurs when lymph builds up in the tissues. It usually appears in parts of the body where a large number of lymph nodes have been removed.
Your legs can get lymphedema if lymph nodes have been removed in your pelvis or groin. Lymphedema is more likely to occur if you have also received radiation therapy to the pelvis.
If you have lymphedema, your healthcare team can suggest ways to reduce the swelling and pain as much as possible and to prevent more lymph from building up. To treat lymphedema, you can lift the limb so that the lymph can flow more easily, exercise, wear compression stockings, and receive regular physiotherapy. You can also ask to be referred to a healthcare professional who specializes in the treatment of lymphedema.
Ascites
Ascites is a buildup of fluid in the abdomen (peritoneal cavity). It occurs when the body produces fluid faster than it can eliminate it. Many women with ovarian cancer have ascites, especially when the disease progresses.
Bowel obstruction
Bowel obstruction occurs when the large intestine (or colon) or small intestine becomes blocked or twisted and its contents cannot flow through it easily. People who have had abdominal surgery are at greater risk of developing intestinal obstruction.
Ovarian cancer often causes intestinal obstruction because the tumor or ascites puts pressure on the intestines. Bowel obstruction due to ovarian cancer forms slowly, taking weeks or months to appear.
Pleural effusion
Pleural effusion is a buildup of fluid in the space (called the pleura) between the outer lining of the lung and the inner lining of the chest wall. It is more likely to occur when the cancer has spread to the area where the lungs are located.
Menopause caused by treatment
Menopause occurs naturally as a woman gets older, usually in her early fifties. It is caused by the decrease in the level of hormones secreted by the ovaries. One of the side effects a woman may experience when receiving treatment for ovarian cancer is premature menopause.
Fertility disorders
The majority of ovarian cancers appear in women who are past their childbearing years, but younger women with ovarian cancer may be concerned about fertility problems they may be experiencing.
Fertility problems can occur after radiation therapy or chemotherapy given to treat ovarian cancer. Most women who have had ovarian cancer surgery are unable to get pregnant because their ovaries have been removed.
To maintain fertility in women who still wish to bear children, treatment for early-stage ovarian cancer may be considered. Before starting any treatment for ovarian cancer, discuss with your healthcare team any side effects that may affect your ability to bear children after treatment and what you can do.
Sexuality
Many women continue to have strong, supportive relationships and satisfying sex lives after ovarian cancer. If you have sexual problems with treatment, there are ways to manage them.
Some side effects of treatment for ovarian cancer can make sex painful or difficult:
vaginal dryness caused by cancer treatments like radiation therapy or surgery
narrowing of the vagina caused by scarring that occurs after radiation therapy to the pelvic area or certain surgeries to the vagina
menopause caused by cancer treatments like radiation therapy or surgery
Some women feel less desire to have sex. It is common to experience a reduced interest in sex at the time of diagnosis and treatment.
When a woman resumes having sex after treatment for ovarian cancer, she may fear that it will be painful or that she may not have an orgasm. The first intimate experiences with another person can be disappointing. It may take a while for a couple to feel comfortable with each other again. Some women and their partners may need counseling to help them cope with these feelings and the effects of cancer treatments on their ability to have sex.
Recidivism
Many women treated for ovarian cancer are concerned about the cancer coming back (coming back). It is important to learn to deal with these concerns in order to maintain a good quality of life.
In addition to the support offered by the treatment team, a mental health professional such as a social worker or counselor can help you learn to live with and cope with a diagnosis of ovarian cancer.
Anxiety and depression
Some women with ovarian cancer have a high degree of anxiety or depression during or after treatment. Anxiety and depression appear to be linked to physical symptoms and the importance of the support they feel they have from loved ones, including caregivers.
You may need help from your healthcare team. You can also ask to be referred to a mental health professional such as a social worker or counselor.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, Mayo Clinic, OCRA, NHS UK, Web MD
Photo credit: Wikimedia Commons
Photo explanation: Diagram showing stage 3A to 3C ovarian cancer.