Understanding Prostate Cancer: Causes, Risk Factors, and Treatment Options
Prostate cancer starts in the cells of the prostate. A cancerous (malignant) tumor is a collection of cancer cells that can invade and destroy the tissues around it. As a cancerous tumor develops (metastasize), it can invade nearby tissues and potentially spread to other parts of the body, posing significant health risks.
The prostate: anatomy and function
The prostate is part of the male reproductive and urinary systems. The size of a walnut, this gland is located just below the bladder in front of the rectum. It surrounds part of the urethra, the duct that carries urine and semen to the end of the penis. The prostate produces mucus and prostatic fluid, which mix with sperm and other fluids to form semen.
Many older men have this disease without knowing it. This type of cancer usually grows slowly and can often be removed completely or treated successfully after being diagnosed. It is common for older men with prostate cancer to die from other causes.
There are also rare types of prostate cancer, such as urothelial carcinoma (also called transitional carcinoma), sarcoma, and small cell carcinoma.
Prostate cancer risk factors
A risk factor is something, like a behavior, substance, or condition that increases your risk for developing cancer. Most cancers are caused by many risk factors, but sometimes prostate cancer develops in men who do not have any of the risk factors described below.
The risk of prostate cancer increases as men get older. The chances of being diagnosed with prostate cancer increase after age 50. Men are most often diagnosed with the disease in their 60s.
Prostate cancer occurs more frequently in men of African descent than in men of other ethnic groups. Men of African descent are also more likely to die from the disease compared to other men. It is not clear what the cause of these differences is.
Family history of prostate cancer
There is convincing evidence that having a family history of prostate cancer increases your risk of developing the disease. This risk is higher if a first-degree relative (eg your father, brother or son) has been diagnosed with prostate cancer. The more first-degree relatives who have prostate cancer, the greater the risk.
The risk of prostate cancer also depends on the age at which your close relative was diagnosed. If that person was diagnosed with this cancer before age 65, your risk of developing prostate cancer is higher than if the diagnosis had been made at a later age.
Possible risk factors
The following factors have been linked to prostate cancer in some way, but there is not enough evidence to say that they are risk factors. More research is needed to clarify the role of these factors in the development of prostate cancer.
Obesity or overweight
Studies show that obesity or being overweight increases the risk of this cancer, and the disease is more likely to have reached an advanced stage at the time of diagnosis. A significant amount of body fat has also been linked to a higher risk of high grade prostate cancer.
Large in adulthood
There is evidence that being tall in adulthood likely increases the risk of this cancer. Several factors that cause tall stature in adulthood, such as genetics and speed of growth in childhood, appear to increase the risk.
Diets rich in dairy products and calcium
There is some evidence that diets high in dairy products and calcium may increase the risk of prostate cancer. Milk, yogurt and cheese are examples of dairy products and foods high in calcium.
Low blood levels of vitamin E or selenium
Studies show that men who have low levels of vitamin E or selenium in their blood may be at higher risk for prostate cancer. However, enough research has not yet been done to conclude that increased intake of vitamin E or selenium through food or supplementation reduces the risk of prostate cancer.
Hereditary genetic mutations
Studies show that certain inherited genetic mutations (changes) can increase the risk of prostate cancer. There are only a very small number of cases of prostate cancer that are linked to inherited genetic mutations.
Two genetic mutations, HOXB13 and BRCA2, are associated with prostate cancer. (The BRCA2 genetic mutation also increases a woman’s risk of breast or ovarian cancer.) Researchers are studying other genetic mutations that may affect prostate cancer risk.
Smoking tobacco
Smoking tobacco may increase the risk of prostate cancer. Some studies also show that smoking tobacco may increase the risk of being diagnosed with rapidly growing (aggressive) or advanced prostate cancer. It is not clear whether smoking affects the incidence of the disease, its prognosis, or both.
High androgen levels
Androgens are male sex hormones that control the growth, development and function of the male reproductive system, which includes the prostate. Testosterone is the main androgen; it is naturally present in the body. It can also be taken to treat certain conditions (treatment of substitution of testosterone).
There is some evidence that high androgen levels in the body are linked to the onset and growth of prostate cancer. More research is needed to understand the long-term effects of the presence of high androgen levels and testosterone replacement therapy.
Inflammation of the prostate
Inflammation of the prostate is called prostatitis. Many studies show that inflammation of the prostate that lasts a long time increases the risk of this cancer. It also makes it grow bigger and spread faster.
Working with certain chemicals
There is evidence to suggest that contact with the following chemicals or substances may increase the risk of prostate cancer.
Pesticides used in agricultural workplaces are associated with a higher risk of prostate cancer. This risk may be even higher for men who have a family history of prostate cancer. Researchers do not know specifically what level of exposure to pesticides or what particular chemicals influence prostate cancer risk.
Cadmium is a metal that causes cancer (carcinogen). Some studies show that men who come in contact with cadmium, in the battery or smelting industry, are at increased risk of developing prostate cancer. Not all studies show such an increased risk.
Chemicals used in the rubber manufacturing industry can increase the risk of this cancer.
Reduce the risk of prostate cancer
You can reduce your risk of this cancer by adopting the following behaviors.
Have a healthy weight
Being overweight and obese can increase your risk for prostate cancer. Eating well and being physically active can help you maintain a healthy weight.
Watch how much dairy products and calcium-rich foods you eat
Diets high in dairy products and calcium may increase the risk of prostate cancer. Milk, yogurt and cheese are examples of dairy products and foods high in calcium. These foods can still be part of a healthy diet. Ask a dietitian how much dairy products and calcium you need to maintain a healthy, balanced diet.
Live smoke-free
If you smoke tobacco, get help to quit. Avoid second-hand smoke.
Protect yourself from pesticides
Avoid or reduce your contact with pesticides. Avoid using pesticides to improve the appearance of green spaces (use of pesticides for cosmetic purposes). If you must use pesticides, try to use the smallest amounts possible. Read the product information and follow the label directions. Wear the recommended protective clothing and equipment when applying pesticides.
Make sure you have completed the necessary training before using pesticides on the job.
Work safely
Follow all workplace health and safety practices, especially if you work in the smelting, battery manufacturing, or rubber industry.
Find out if your risk of prostate cancer is high
Some men, including those with a family history of prostate cancer, may have a higher than average risk of developing the disease. Discuss your risk with your doctor. If it is above average, you may need to see your doctor more often to check for prostate cancer. Your doctor will tell you which tests to take and how often.

In anatomy the lobes are clearly defined anatomical divisions or extensions of organs. Photo source: Steven Fruitsmaak – Wikipedia
Stages of prostate cancer
Staging describes or categorizes cancer based on how much cancer is in the body and where it was initially diagnosed. This is often referred to as the extent of cancer. Information from tests is used to find out how big the tumor is, what parts of the organ have cancer, if the cancer has spread from where it started and where it has spread. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The most frequently used staging system for prostate cancer is the TNM classification. In the case of prostate cancer, there are 4 stages. For stages 1 to 4, we often use the Roman numerals I, II, III and IV, but, in order to make the text clearer, we will use the Arabic numerals 1, 2, 3 and 4. In general, more the higher the stage number, the more the cancer has spread. Talk to your doctor if you have questions about staging.
When doctors describe the stage, they often use the words localized, locally advanced, or metastatic.
Localized means that the cancer is only found in the prostate. It has not invaded nearby tissues and has not spread to distant parts of the body. Localized this cancer has stages 1 and 2.
Locally advanced means that the prostate cancer has passed through the envelope of the prostate (called the capsule) to invade nearby tissues. This cancer is said to be locally advanced if it is stage 3 or 4 and if it has not spread to distant parts of the body (no metastases).
Metastatic means the cancer has spread beyond the tissues around the prostate to other parts of the body.
Doctors can also use the words local, regional or distant. Local means the cancer is only in the prostate and has not spread to other parts of the body. Regional means near or around the prostate. Distant means in a part of the body farther from the prostate.
The following information is about the staging of adenocarcinoma, which accounts for 95% of prostate cancer cases. The staging of other types of this cancer is different. Urothelial carcinoma is a type of cancer that starts in the cells that line the urethra, including the part that goes through the prostate (called the prostatic urethra). The staging of urothelial carcinoma of the prostatic urethra is similar to that of cancer of the renal pelvis and ureter. Find out more about urothelial carcinoma and the staging of cancer of the renal pelvis and ureter.
TNM classification descriptions
T describes how much of the prostate has cancer and whether doctors can feel it or see it with imaging tests. T also indicates whether the tumor has passed through the prostate and invaded the tissues surrounding it. T is usually graded from 1 to 4. A higher number means that the tumor occupies a greater proportion of the prostate or that it has passed through the prostate to invade nearby tissues.
N describes the spread of cancer to lymph nodes near the prostate. N0 means the cancer has not spread to any nearby lymph nodes. N1 means the cancer has spread to nearby lymph nodes.
M describes the spread of cancer to other parts of the body. M0 means the cancer has not spread to other parts of the body. M1 means the cancer has spread to other parts of the body.
Find out more about cancer staging
Stage 1 (T1 or T2a, N0, M0)
Cancer may have been detected when prostate tissue was taken for another condition, such as benign prostatic hyperplasia. Cancer may also have been detected during a needle biopsy.
OR
The tumor is located in a single lobe of the prostate and occupies half or less than half of that lobe (T2a).
Stage 2 (T2b or T2c, N0, M0)
The tumor occupies more than half of a lobe (T2b) or it affects both lobes (T2c) of the prostate.
Stage 3 (T3 or T4, N0, M0)
The tumor passed through the capsule and invaded either the lower part of the bladder (called the bladder neck) or one or both seminal vesicles (glands above the prostate) (T3).
OR
The tumor has attached or spread to one or more of the following structures:
- rectum
- external anal sphincter
- pelvic floor elevator muscles
- basin wall
Stage 4 (any T, N1, M0 or any T, N0, M1)
The cancer has spread to nearby lymph nodes (N1) or to parts of the body far from the tumor, such as bones (M1). This cancer that has spread to parts of the body removed from the tumor is called metastatic prostate cancer.
Recurrent prostate cancer
If this cancer comes back, the cancer comes back after treatment. If it reappears where it first started, it is called a local recurrence. If it reappears in tissues or lymph nodes near where it first started, it is called a regional recurrence. It can also reappear in another part of the body: this is called a recurrence or distant metastasis.
Recurrent prostate cancer is also diagnosed when the level of prostate specific antigen (PSA) starts to rise rapidly after the initial treatment without there being any other signs of cancer. This is called a biochemical recurrence of prostate cancer.
If prostate cancer spreads
Cancer cells can spread from the prostate gland to other parts of the body. This spread is called metastasis.
Understanding how a type of cancer tends to grow and spread helps your healthcare team plan for your future treatment and care. If this cancer spreads, it can spread to the following structures:
- bladder
- urethra
- ejaculatory ducts (ducts connecting the seminal vesicles to the part of the urethra that passes through the prostate)
- seminal vesicles (glands on either side of the prostate)
- rectum
- basin wall
- lymph nodes located in the pelvis
- lymph nodes located outside the pelvis
- bone
- lungs
- liver
- brain
Tumor Markers: What They Are and How They’re Used to Diagnose and Monitor Cancer
Prognosis and survival for prostate cancer
If you have this cancer, you may be wondering about your prognosis. Prognosis is the act by which the doctor best judges how the cancer will affect a person with cancer. The prognosis and survival depend on many factors. Only a doctor who is familiar with your medical history, the type, stage and characteristics of the cancer you have, the treatments chosen and the response to the treatment can look at all of this data together with the survival statistics to arrive at an understanding. prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person affected that the doctor takes into account when making a prognosis.
The following are prognostic factors for this cancer.
Stadium
A lower stage prostate cancer at the time of diagnosis has a more favorable prognosis. The prognosis for cancer that has not spread outside the prostate at the time of diagnosis is better than for cancer that has.
Grade
This cancer with a Gleason score below 7 has a more favorable prognosis. When the Gleason score is over 7, prostate cancer is considered high grade, which means cancer cells grow quickly and are more likely to spread.
Prostate specific antigen (PSA) level
Some research indicates that higher than normal prostate specific antigen (PSA) levels can have a poor prognosis because high PSA levels are associated with an increased risk of prostate cancer spreading.
APS doubling time
The APS doubling time measures the time it takes for the APS rate to double. For example, a 3-year APS doubling time means that on average, the APS rate doubles every 3 years. The APS doubling time helps doctors determine whether prostate cancer is aggressive – that is, whether it tends to grow quickly and spread. A shorter doubling time is associated with a poorer prognosis.
Smoking
There is some evidence that men who smoke at the time of diagnosis are more likely to have a biochemical recurrence (also called biochemical failure) and die from this cancer than men who do not smoke. A biochemical recurrence means that the level of PSA starts to increase after treatment without there being any other signs of cancer.
Levels of certain chemicals in the blood
Changes in the level of certain chemicals in the blood can have a poor prognosis in men with metastatic hormone-resistant prostate cancer:
- high level of alkaline phosphatase
- low hemoglobin
- low albumin
- high level of lacticodehydrogenase
Genetic signatures
The gene expression profile is a way to analyze many genes at once to find out which are active and which are not. Doctors have found several abnormal genetic patterns (genetic signatures) in people with this cancer. These genetic signatures help them make a prognosis. Some genetic signatures are associated with a better prognosis and better response to treatment, while other signatures are associated with a poorer prognosis.
Using nomograms to assess prognosis
Nomograms are predictive statistical models that assess the probable prognosis taking into account stage, Gleason score, PSA level, pathology reports written after biopsies, use of hormone therapy, radiation dose and other information specific to the affected man, such as his age or previous treatments.
Nomograms used to establish the prognosis of prostate cancer include the following.
Prostate Cancer Risk Assessment Nomogram (CAPRA)
Doctors use the Cancer of the Prostate Risk Assessment (CAPRA) nomogram to help them estimate the risk of cancer spreading, estimate the risk of a man dying from cancer prostate cancer and in making treatment decisions.
This nomogram is based on the following elements:
- PSA (prostate-specific antigen) tumor marker rate in the blood
- Gleason’s rating (score rates the aggressiveness of prostate cancer cells on a scale of 6 to 10, helping guide treatment and predict prognosis)
- percentage of biopsy samples with cancer present
- stage of cancer at diagnosis (clinical stage)
- age at diagnosis
- Partin tables
Partin’s tables are nomograms that help doctors estimate the risk of cancer spreading before surgery to remove the prostate and make decisions about the trait.
Tumor Markers: What They Are and How They’re Used to Diagnose and Monitor Cancer
TNM prognostic groups
TNM prognostic grouping for this cancer is based on the stage, PSA level and Gleason score. This grouping is more accurate in predicting a prognosis than TNM staging alone. Men in group I have the best outlook and chance that their cancer can be successfully treated without the cancer coming back (recurring). Men in group II have the next best prognosis, followed by men in group III. Although men in group IV have the poorest prognosis compared to the other 3 groups, there may still be treatment options to control their cancer, improve their quality of life and prolong their survival.
| Group | Tumour details (T) | Spread to lymph nodes (N) | Spread to other parts of the body (M) | PSA level (ng/mL) | Gleason score |
|---|---|---|---|---|---|
| I | T1 | N0 | M0 | less than 10 | 6 or less |
| T2a | N0 | M0 | less than 10 | 6 or less | |
| IIA | T1 | N0 | M0 | less than 20 | 7 |
| T1 | N0 | M0 | 10 or more but less than 20 | 6 or less | |
| T2a or T2b | N0 | M0 | less than 20 | 7 or less | |
| IIB | T2c | N0 | M0 | any PSA level | any Gleason score |
| T1, T2a, T2b or T2c | N0 | M0 | 20 or greater | any Gleason score | |
| T1, T2a, T2b or T2c | N0 | M0 | any PSA level | 8 or more | |
| III | T3 | N0 | M0 | any PSA level | any Gleason score |
| IV | T4 | N0 | M0 | any PSA level | any Gleason score |
| any T | N1 | M0 | any PSA level | any Gleason score | |
| any T | any N | M1 | any PSA level | any Gleason score |
Risk of prostate cancer recurrence
Doctors may classify prostate cancer into groups based on the risk of the cancer coming back (recurring) after treatment. They use these risk levels to help them develop treatment plans. Men in the high-risk group are usually offered aggressive treatment. Those in the low-risk group may be offered active surveillance without immediate treatment.
Active Cancer Surveillance and Visits | Monitoring and Follow-up for Cancer Survivors
The risk level is based on the:
- tumour (T)
- prostate-specific antigen (PSA) level
- Gleason score
| Risk level | Tumour details (T) | PSA level (ng/mL) | Gleason score |
|---|---|---|---|
| low risk | T1 or T2a | less than 10 | 6 or less |
| intermediate risk | T2b or T2c | 10 to 20 | 7 |
| high risk | T3 or T4 | greater than 20 | 8, 9 or 10 |
Survival statistics for prostate cancer
Survival statistics for this cancer are very general estimates and must be interpreted very carefully. Because these statistics are based on the experience of groups of people, they cannot be used to predict a particular person’s chances of survival. In general, most men diagnosed with prostate cancer do not die from the disease itself and will die from other causes.
There are many different ways to measure and report cancer survival statistics. Your doctor can explain the statistics for prostate cancer and what they mean to you.
Net survival
Net survival represents the probability of surviving cancer in the absence of other causes of death. It is used to give an estimate of the percentage of people who will survive their cancer.
For example in Canada, the 5-year net survival for prostate cancer is 93%. This means that about 93% of men diagnosed with prostate cancer will survive for at least 5 years after their diagnosis.
Survival by stage
Survival varies with each stage of this cancer. The grade of prostate cancer is also a strong predictor for survival.
Generally, the earlier this cancer is diagnosed and treated, the better the outcome. Because prostate cancer tends to grow slowly, it can often be successfully treated. In addition, there are many treatments available for prostate cancer and it often responds well to treatment.
Advanced and recurrent this cancers and castrate-resistant prostate cancer (prostate cancer that doesn’t respond to or comes back after hormonal therapy) can be difficult to treat because they do not respond well to some treatments.
Survival for stage of this cancer is reported as 5-year relative survival. Relative survival looks at how likely people with cancer are to survive after their diagnosis compared to people in the general population who do not have cancer but who share similar characteristics (such as age and sex).
There are no specific Canadian statistics available for the different stages of prostate cancer. The following information comes from a variety of sources. It may include statistics from other countries that are likely to have similar outcomes as in Canada.
| Stage | 5-year relative survival |
|---|---|
| 1, 2 or 3 | nearly 100% |
| 4 (when the cancer hasn’t spread to other parts of the body) | nearly 100% |
| 4 (when the cancer has spread to other parts of the body) | 28% |
Questions about survival
Talk to your doctor about your prognosis. A prognosis depends on many factors, including:
- your health history
- the type of cancer
- the stage
- certain characteristics of the cancer
- the treatments chosen
- how the cancer responds to treatment
Only a doctor familiar with these factors can put all of this information together with survival statistics to arrive at a prognosis.
Prostate cancer treatment options
If you have this cancer, your healthcare team will create a treatment plan especially for you. This plan will be based on your condition and cancer-specific information.
When your healthcare team decides what treatments to offer for prostate cancer, they take the following into consideration:
- the type and stage of cancer
- Gleason’s grade or score (score rates the aggressiveness of prostate cancer cells on a scale of 6 to 10, helping guide treatment and predict prognosis)
- possible side effects of treatments
- your personal preferences
- your overall health
- your age and life expectancy
Doctors may also classify this cancer based on its risk of recurrence (coming back) after treatment. Aggressive treatment is usually offered to men at high risk. Those at low risk may be offered active surveillance without immediately receiving treatment. Find out more about the risk of prostate cancer coming back.
You may be offered one of the following treatments (or a combination of them) for this cancer.
Active surveillance
Active surveillance means that the healthcare team is watching you for signs or symptoms that indicate the cancer is progressing. You will meet with your doctor and have tests every 3 to 6 months. You will be started on treatment as soon as you see signs that the disease is starting to develop or spread (this is called disease progression).
Active Cancer Surveillance and Visits | Monitoring and Follow-up for Cancer Survivors
Surgery
Depending on the stage of the cancer and your condition, one of the following types of surgery may be done.
Cancer Surgery (Operation): Understanding Types, Risks, and Recovery
Radical prostatectomy
A radical prostatectomy removes the prostate and some of the surrounding tissue, including the seminal vesicles. This is the most common type of surgery used to treat prostate cancer.
There are different types of radical prostatectomy, including:
- radical retropubic prostatectomy
- radical perineal prostatectomy
- laparoscopic radical prostatectomy
- robotic radical prostatectomy
- radical prostatectomy with preservation of the nerves
Transurethral resection of the prostate (TURP)
In a transurethral resection of the prostate (TURP), part of the prostate is removed through the urethra. The goal of this surgery is to relieve urinary problems caused by an enlarged prostate which is putting pressure on the urethra. It can also be used to reduce the size of the tumor before starting other treatments. TURP is used to treat men with advanced prostate cancer or those who are not healthy enough to undergo radical prostatectomy.
Cryosurgery
Cryosurgery uses extreme cold (liquid nitrogen or liquid carbon dioxide) to freeze and destroy abnormal cells. For the moment, cryosurgery remains an experimental treatment for prostate cancer. Doctors sometimes use it to treat prostate cancer that comes back (comes back) after radiation therapy.
Pelvic lymph node dissection
A pelvic lymph node dissection (also called pelvic lymphadenectomy) removes the lymph nodes in the pelvis. This procedure can be performed at the same time as a radical prostatectomy.
Radiotherapy
Radiation therapy is a common treatment for prostate cancer. Different techniques are used, including external beam radiation therapy, brachytherapy and systemic radiation therapy.
Hormone therapy
Hormone therapy is most often used to treat advanced prostate cancer or prostate cancer that comes back (comes back) after other treatments. It can be given at the same time as radiotherapy. Lowering androgen levels to slow cancer growth, typically used for advanced or recurrent prostate cancer.
Chemotherapy
Chemotherapy may be used for advanced prostate cancer. It can be used to treat prostate cancer that does not respond to hormone therapy or that comes back (comes back) after being treated with hormone therapy (hormone-resistant prostate cancer). In men with metastatic prostate cancer, chemotherapy is also sometimes given at the same time as hormone therapy. Find out more about chemotherapy.
High Intensity Focused Ultrasound (HIFU)
High Intensity Focused Ultrasound (HIFU) treatment employs focused ultrasound to create intense heat that destroys cancer cells. At the moment, HIFU are an experimental treatment for prostate cancer. Doctors sometimes use it to treat prostate cancer that comes back after radiation therapy.
Corticosteroids
Corticosteroids are steroid hormones that work like anti-inflammatory drugs by reducing swelling and the immune response (the reaction of the immune system to the presence of foreign substances in the body). Theyhave sometimes been given at the same time as chemotherapy to make it more effective and to reduce side effects. They can also be used on their own if a person is too sick to receive chemotherapy. Corticosteroids can help slow the growth of prostate cancer cells and relieve symptoms such as pain.
Prednisone and dexamethasone (Decadron, Dexasone) are the most common corticosteroids used to treat this cancer.
If you cannot or do not want to be treated for cancer
You may want to consider care that aims to make you feel better without treating the cancer itself, perhaps because cancer treatments no longer work, are no longer likely to improve your condition, or their side effects are difficult to tolerate. There may be other reasons why you cannot or do not want to be treated for cancer.
Talk to members of your healthcare team. They can help you choose advanced cancer care and treatment.
Monitoring
Follow-up after treatment is an important part of caring for people with cancer. You will need to have regular follow-up visits, especially during the first five years after completing treatment. These visits will allow the healthcare team to monitor your progress and to know how you are recovering from treatment.
Clinical tests
Numerous clinical trials in prostate cancer are available in certain countries and are accepting participants. Clinical trials aim to find better methods of preventing, detecting and treating cancer. Find out more about clinical trials.
Conclusion
Prostate cancer remains a significant health concern for men worldwide. Understanding its causes, risk factors, and treatment options is essential for early detection and effective management. By adopting healthy lifestyle choices and seeking regular medical check-ups, individuals can reduce their risk and improve their chances of successful outcomes in case of diagnosis.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, Web MD, U.S. Department of Health & Human Services, Medline Plus, Mayo Clinic
Photo credit: Wikimedia Commons
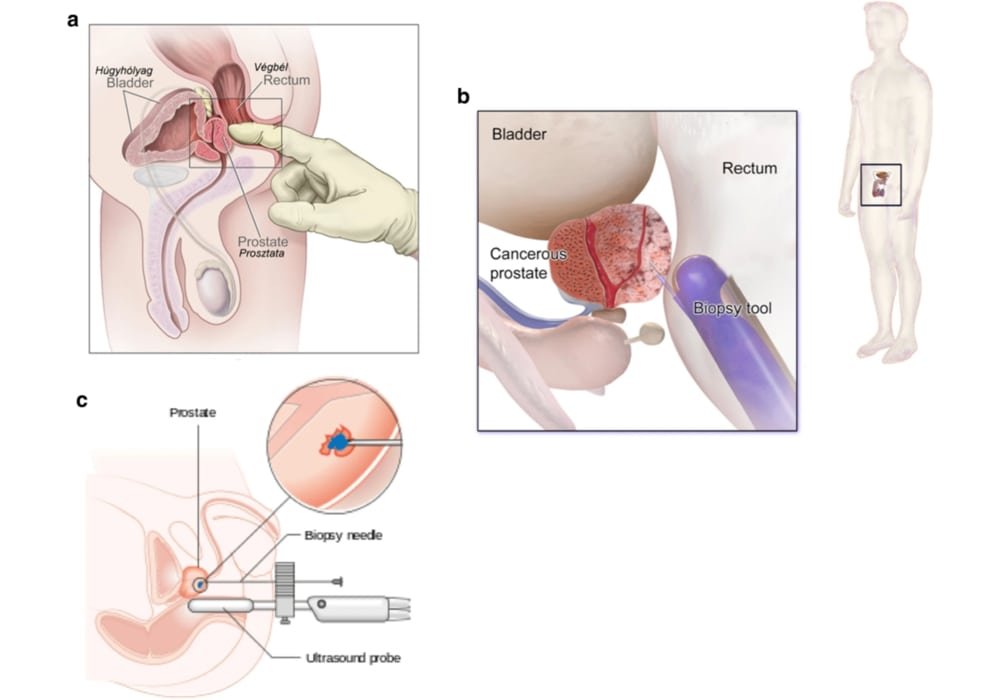
Photo explanations: Diagnosis Method of Prostate Cancer.