What is esophageal cancer?
Esophageal cancer starts in the cells of the esophagus. Cancerous (malignant) tumor is a group of cancer cells that can invade and destroy nearby tissue. The tumor can also spread (metastasize) to other parts of the body.
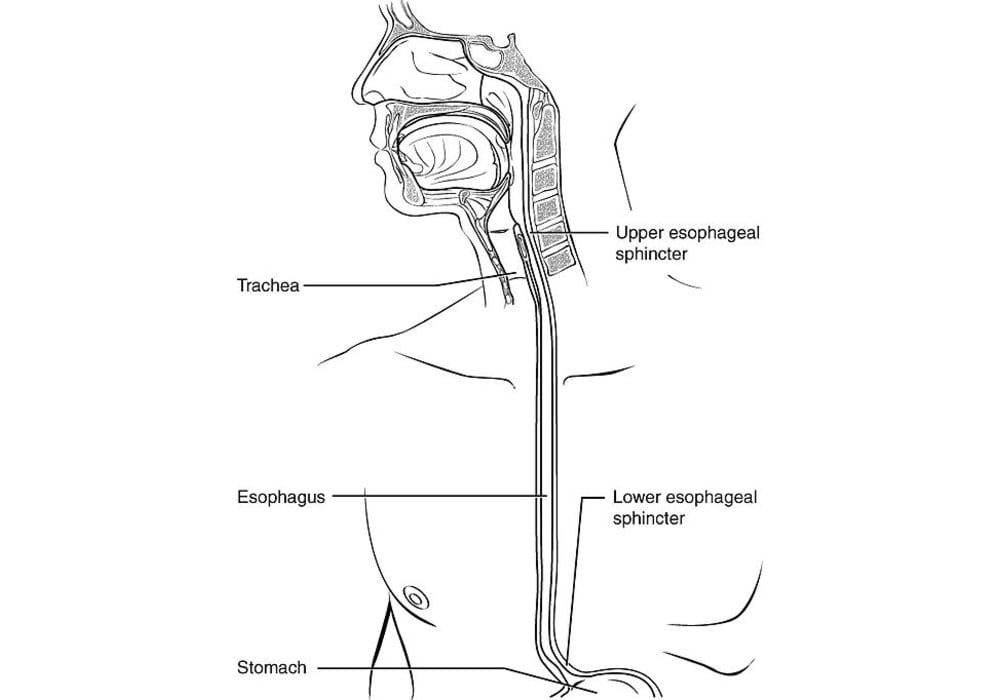
The esophagus is part of the digestive system. It is a component of the digestive tract, which is the tube from the mouth and down to the anus. The digestive tract includes the esophagus, stomach, small intestine, large intestine, and other organs.
swallowed to the stomach thanks to peristalsis, the sequential wave of its musculature. It is 25 to 30 cm long in adult humans and 5 cm in newborns.
The most common type is squamous cell carcinoma of the esophagus, often associated with alcohol and tobacco poisoning and / or drinking too hot drinks. The second most common type is adenocarcinoma.
Types
There are 2 types of cancer (esophageal squamous cell carcinoma, and oesophageal adenocarcinoma, the former more suggestive of squamous carcinomas of other organs than esophageal adenocarcinomas).
Adenocarcinoma
Esophageal adenocarcinoma starts in the glandular cells of the tissues lining the esophagus. It is the most common type of esophageal cancer in developed Western countries like Canada and the United States. Adenocarcinoma is usually found in the lower part of the esophagus, inside tissue that has been damaged in people with Barrett’s esophagus. This tumor often spreads to the stomach.
Squamous cell carcinoma
Squamous cell carcinoma starts in the flat cells of the tissue lining the esophagus. The highest rates of squamous cell carcinoma of the esophagus are found in parts of China, Iran, South America, France and Africa. This tumor is usually found in the middle or upper part of the esophagus.
Rare esophageal tumors
The following cancerous tumors of the esophagus are rare:
- leiomyosarcoma (rare type of cancer that affects smooth muscle tissue)
- gastrointestinal stromal tumour (GIST)
- neuroendocrine tumour (NET)
Risk factors for esophageal cancer
A risk factor is something, like a behavior, substance, or condition that increases your risk for developing cancer. Most cancers are caused by many risk factors, but esophageal cancer can develop in people who do not have any of the risk factors described below.
The most common types of esophageal cancer are adenocarcinoma and squamous cell carcinoma. They have some risk factors in common, but other risk factors are only linked to adenocarcinoma or squamous cell carcinoma of the esophagus.
Men are more likely than women to develop esophageal cancer. Most people diagnosed with esophageal cancer are men over the age of 60. The highest rates of squamous cell carcinoma of the esophagus are found in parts of China, Iran, South America, France and Africa, and the incidence is declining worldwide. In contrast, the incidence of esophageal adenocarcinoma is increasing, especially in middle- and high-income countries. Low socioeconomic status increases the risk of esophageal cancer, especially squamous cell carcinoma.
Barrett’s esophagus is the most common precancerous condition of the esophagus. It’s not cancer, but it can sometimes turn into esophageal cancer if left untreated. Some of the risk factors for esophageal cancer can also cause Barrett’s esophagus.
Risk factors are usually ranked from most important to least important. But in most cases, it is impossible to rank them with absolute certainty.
Risk factors:
- Tobacco
- Alcohol
- Betel quid
- Gastroesophageal reflux disease (GERP)
- Overweight or obese
- Consumtion of very hot drinks
- Tylosis
- Achalasia
- Plummer-Vinson syndrome
- Chemical damage to the esophagus
- History of upper respiratory cancer
- Exposure to ionizing radiation
There is convincing evidence that the above factors increase your risk for esophageal cancer.
Diagnosis of esophageal cancer
Diagnosis is the process of identifying the cause of a health problem. The diagnostic process for esophageal cancer usually begins with a visit to your family doctor. Your doctor will ask you about your symptoms and may do a physical exam. Based on this information, your doctor may refer you to a specialist or order tests to check for esophageal cancer or other health problems.
The diagnostic process can seem long and overwhelming. It’s okay to worry, but try to remember that other medical conditions can cause esophageal cancer-like symptoms. It is important that the healthcare team rule out any other possible cause of the condition before making a diagnosis of esophageal cancer.
The following tests are usually used to rule out or diagnose esophageal cancer. Many tests that can diagnose cancer are also used to determine its stage, that is, how far the disease has progressed. Your doctor may also give you other tests to check your general health and help plan your treatment.
Health history and physical examination
Your health history consists of a checkup of your symptoms, risk factors, and any medical events and conditions you may have had in the past. Your doctor will ask you questions about your history:
- symptoms that suggest cancer of the esophagus, such as difficulty swallowing;
- gastroesophageal reflux disease (GERD);
- Barrett’s esophagus;
- smoking and alcohol consumption;
- weightloss.
Your doctor may also ask you questions about your family history:
- esophageal cancer;
- risk factors for esophageal cancer;
- other cancers.
The physical exam allows your doctor to look for any signs of esophageal cancer. During the physical examination, your doctor may:
- check if your voice is hoarse;
- feel the lymph nodes above your collarbones and in your neck to see if they are swollen;
- feel your abdomen to see if any organs are swollen or if fluid has accumulated in them (ascites);
- check your spine to see if your vertebrae are painful.
Esophageal-duodenal transit
During esophageal-duodenal transit, special fluids are used to cover the inside of the organs and clearly reveal their outline on x-ray. You swallow the liquid, then the technician takes x-rays of your upper digestive tract including the esophagus, stomach, and upper segment of the small intestine.
Esophageal transit is often the first test used to diagnose esophageal cancer. It can reveal:
- a lesion on the surface of the esophagus (ulcer);
- narrowing (stenosis) of the esophagus;
- the location and overall size of the tumor in the esophagus;
- an abnormal opening of the esophagus into the trachea (tracheoesophageal fistula);
- your ability to swallow;
- if the cancer has spread to the stomach.
Upper gastrointestinal endoscopy
Upper gastrointestinal endoscopy examines the upper digestive tract, including the esophagus, stomach, and the first part of the small intestine (duodenum). An endoscope is then used, which is a flexible tube with a lumen and a lens at one end. The doctor inserts the endoscope into your mouth and takes it down your throat to the esophagus. Before the procedure, the back of your throat is sprayed with a local anesthetic to numb it. You may also be given intravenous (IV) medicine to help you relax and stay calm during the test.
Upper gastrointestinal endoscopy is used to:
- examine the esophagus, stomach and duodenum for bleeding, ulcers, tumors, inflammation or narrowing;
- take tissue samples that will be analyzed in the laboratory (biopsy);
- widen, or dilate, the esophagus if there is a narrowing;
- insert a narrow tube called a stent into the esophagus if it is blocked by a tumor.
Echoendoscopy
In an ultrasound, high-frequency sound waves are used to produce images of body structures. Endoscopic ultrasound (EE) uses an endoscope and an ultrasound probe. It can provide detailed information about the location, size and depth of the tumor. It can also tell doctors if the cancer has spread to lymph nodes or nearby tissue.Often done EE at the same time as an upper gastrointestinal endoscopy.
Biopsy
During a biopsy, the doctor removes tissue or cells from the body for analysis in the laboratory. The laboratory report confirms whether or not there are cancer cells in the sample.
In an endoscopic biopsy, tissue is removed from the esophagus using an endoscope during an upper gastrointestinal endoscopy or endoscopic ultrasound (EA).
A fine needle biopsy (BAF) can be done through the wall of the esophagus to check for cancer in nearby lymph nodes.
When brushing, a needle or brush is used to remove cells from an area of the abdomen that looks abnormal or is suspicious.
CT scan
A computed tomography (CT) scan uses special x-ray machines to produce 3-dimensional and cross-sectional images of the body’s organs, tissues, bones and blood vessels. A computer assembles the photos into detailed images.
CT scans the chest and abdomen to determine the size and location of the tumor in the esophagus to help determine its stage. It is also used to find out if the cancer has spread to nearby lymph nodes, liver, lungs or adrenal glands. CT also helps guide a biopsy needle when you want to remove tissue from abnormal or suspicious lymph nodes.
CT is more effective at determining the stage of advanced esophageal cancer than at detecting a small, early tumor in the esophagus.
Positron emission tomography
A positron emission tomography (PET) scan uses a radioactive material called a radiopharmaceutical to detect changes in the metabolic activity of body tissues. A computer analyzes patterns of radioactivity distribution and produces 3-dimensional, color images of the region under examination.
A PET is used to look for very small tumors in the chest or abdomen that may have spread from cancer of the esophagus. A PET also shows how well an esophageal cancer responds to chemotherapy or radiation therapy.
PET may be associated with CT (PET / CT). Newer devices allow PET to be done at the same time as CT. PET / CT provides more detailed information about body structures that are sometimes difficult to see with PET alone.
Laparoscopy
Laparoscopy is a procedure in which a laparoscope (a thin, tube-shaped instrument with a lumen and a lens) is used to examine or treat organs in the abdomen and pelvis. It allows doctors to examine and remove internal organs through several small incisions. Doctors may also take samples during the laparoscopy (laparoscopic biopsy).
Laparoscopy is used to accurately determine the stage of esophageal cancer so that doctors can plan treatment. It can be used to detect cancer that has spread to other parts of the abdomen and was not seen on a PET or CT scan.
Complete blood count
The complete blood count (CBC) is used to assess the quantity and quality of white blood cells, red blood cells and platelets. A BSC is done to check for anemia caused by bleeding that has lasted a long time (chronic). An SCF can also be done to obtain baseline values against which the results of blood tests performed during and after treatment can be compared to monitor the effects of treatments that may reduce the number of blood cells.
Blood biochemical analyzes
A blood chemistry test measures the level of chemicals in the blood. It makes it possible to evaluate the quality of functioning of certain organs and also to detect anomalies.
Liver function tests may be done to determine the stage of esophageal cancer. These tests measure the level of lacticodehydrogenase (LDH), alanine aminotransferase (ALT), aspartate transaminase (AST), alkaline phosphatase (AP) and bilirubin so that you know how well the liver is functioning. A rise in the level of these enzymes can mean that the cancer has spread to the liver. A rise in BP levels can also mean that the cancer has spread to the bones.
HER2 status analysis
ErbB2 is better known as HER2, or HER2 / neu. HER2 stands for human epidermal growth factor receptor 2. This is a gene that has undergone a change (mutation) and can therefore promote the growth of a tumor, called an oncogene. Testing for HER2 status is used to see if cells are making more HER2 protein than normal (overexpression).
Esophageal tumors present at the junction between the esophagus and the stomach, the esophagogastric (OG) junction, are tested for the HER2 status. This information will help your healthcare team determine which treatments will work best for you.
Stages of esophageal cancer
Staging describes or categorizes cancer based on how much cancer is in the body and where it was initially diagnosed. This is often referred to as the extent of cancer. Information from tests is used to find out how big the tumor is, which parts of the esophagus have cancer, whether the cancer has spread from where it originated, and where it has spread. Your healthcare team uses the stage to plan your treatment and predict the outcome (your prognosis).
The staging of esophageal cancer includes cancer of the esophagus but also cancer of the esophagogastric (OG) junction, where the esophagus meets the stomach.
Adenocarcinoma and squamous cell carcinoma are the most common types of esophageal cancer. Their stages vary a bit, as shown below.
The most commonly used staging system for esophageal cancer is the TNM staging system. For esophageal cancer there are 5 stages, stage 0 followed by stages 1 to 4. For stages 1 to 4, the Roman numerals I, II, III and IV are often used. But in order to make the text clearer, we will use the Arabic numerals 1, 2, 3 and 4. In general, the higher the stage number, the more cancer has spread. Talk to your doctor if you have questions about staging.
When doctors describe the stage, they may use the words early, locally advanced, or metastatic. Early means the cancer is only found in the esophagus and has not spread to other parts of the body. Locally advanced means near or around the esophagus, including neighboring lymph nodes. Metastatic means in a part of the body farther from the esophagus.
The stages of esophageal cancer also depend on the grade. The grade describes how much cancer cells differ in appearance from normal cells, how quickly they grow and divide, and how likely they are to spread.
Grades of esophageal cancer
To determine the grade of esophageal cancer, the pathologist examines a sample of tissue taken from the tumor under a microscope. The pathologist assigns a grade of 1 to 3 to cancer of the esophagus. The lower this number, the lower the rank.
The grade is defined by the appearance and behavior of cancer cells compared to normal cells. The word differentiation is used to refer to how different cancer cells are.
Low-grade cancer cells are well differentiated or moderately differentiated. They look and behave very much like normal cells. They tend to grow slowly and are less likely to spread.
High-grade cancer cells are poorly differentiated or undifferentiated. Their appearance and behavior are less normal, or more abnormal. They tend to grow faster and are more likely to spread.
Knowing the grade can give your healthcare team an idea of how quickly cancer can grow and how likely it is to spread. It helps him plan your treatment. The grade can also help the healthcare team predict how you might respond to treatment.
If esophageal cancer spreads
Cancer cells can spread from the esophagus to other parts of the body. This spread is called metastasis.
Understanding how a type of cancer usually grows and spreads helps your healthcare team plan your treatment and future care.
If esophageal cancer spreads, it can spread to the following parts of the body:
- lymph nodes around the esophagus;
- lymph nodes in the neck or upper chest;
- lymph nodes in the lower chest or around the stomach;
- lymph nodes in the abdomen;
- trachea;
- vocal cords;
- main artery that leads to the heart (aorta);
- pericardium;
- stomach;
- liver;
- adrenal glands;
- lungs;
- bone;
- brain.
Prognosis and survival for esophageal cancer
If you have esophageal cancer, you may be wondering about your prognosis. A prognosis is the act by which the doctor best assesses how cancer will affect a person and how they will respond to treatment. The prognosis and survival depend on many factors. Only a doctor who is familiar with your medical history, the type of cancer you have, the stage and other characteristics of the disease, the treatments chosen and the response to treatment can review all of this data together with survival statistics. to arrive at a prognosis.
A prognostic factor is an aspect of the cancer or a characteristic of the person (such as their age or general health) that the doctor takes into account when making a prognosis. A predictor factor influences how cancer responds to a certain treatment. Prognostic and predictor factors are often discussed together and both play a role in the choice of treatment plan and in establishing the prognosis.
The following are the prognostic factors for esophageal cancer.
Stadium
The most important prognostic factor for esophageal cancer is the stage of the tumor at diagnosis. Esophageal cancer detected at an early stage has a better outcome than esophageal cancer detected at an advanced stage.
An esophageal tumor seen only in the lining of the esophagus has a better prognosis than a tumor that has passed through the muscle wall of the esophagus or has spread to other organs.
Tumor size
A small tumor has a better prognosis than a large tumor.
Spread of cancer to the lymph nodes
The lower the number of lymph nodes affected by cancer, the better the prognosis.
Spread of cancer to distant organs
Esophageal cancer that has spread to organs in other parts of the body has a poorer prognosis.
Complete surgical removal of cancer
The amount of cancer that is left after surgery is called residual disease. The absence of residual disease results in a better prognosis than if there is still some cancer left after the operation.
Cancer that responds to neoadjuvant therapy
Esophageal cancer that responds to neoadjuvant therapy is more likely to be completely removed with surgery. Therefore, cancer that responds to neoadjuvant therapy has a better prognosis than cancer that does not.
Treatments for esophageal cancer
If you have esophageal cancer, your healthcare team will make a treatment plan just for you. It will be based on your health and specific cancer information. When your healthcare team decides which treatments to offer you for esophageal cancer, they take the following into consideration:
- the stage of the cancer;
- where the tumor is in the esophagus (its location);
- the type of esophageal cancer;
- your overall health;
- your personal preferences.
Before your healthcare team decides which treatments to offer you, they will assess your overall health to see what types of treatments you can tolerate. She will examine your lungs and heart to make sure they are working properly.
People diagnosed with esophageal cancer often have difficulty eating. Your healthcare team will assess your weight and your ability to eat. You may need nutritional supplements, a feeding tube, or intravenous feeding for a few days before and after surgery to gain weight and improve your nutritional status and health. You may also need to take antibiotics to prevent or treat infections if malnutrition has weakened your immune system.
If you smoke, it is very important to give up smoking before treatment. Smokers are more likely to have side effects and complications during treatment for esophageal cancer. Treatment may not be as effective in smokers as it is in non-smokers.
You may be offered one or more of the following treatments for esophageal cancer.
Surgery
If you are healthy, and the tumor can be completely removed, you will be offered surgery to treat esophageal cancer.
Esophagectomy removes part or all of the esophagus, as well as the nearby lymph nodes. Sometimes part of the stomach is also removed.
Chemotherapy and chemoradiotherapy
Chemotherapy can be used to treat esophageal cancer. Although only chemotherapy can be used, most often radiation therapy is also given at the same time (chemoradiotherapy). Some chemotherapy drugs make radiation therapy more effective.
Chemoradiation therapy can be given:
- before surgery (neoadjuvant chemoradiotherapy);
- after surgery (adjuvant chemoradiotherapy).
You can only give chemotherapy:
- as the main treatment if you are not healthy enough to have surgery, or if you do not want to have surgery or chemoradiation;
- as a treatment for recurrent or advanced esophageal cancer that cannot be treated with surgery or radiation
- therapy.
Radiotherapy
Radiation therapy may be used to treat esophageal cancer. It is usually given at the same time as chemotherapy (chemoradiation).
Radiation therapy may only be used as treatment for esophageal cancer if you are not healthy enough to have surgery or chemoradiotherapy, or if you do not want to receive any of these treatments. .
Radiation therapy may also be given only to treat symptoms of esophageal cancer that is advanced, or to treat esophageal cancer that has come back (comes back) after treatment.
Targeted treatment
Targeted therapy uses drugs or other substances to target specific molecules (usually proteins) that help cancer cells grow while limiting damage to normal cells.
Targeted drugs are used to treat locally advanced or metastatic adenocarcinoma located at the esophagogastric (OG) junction. They are usually combined with chemotherapy.
Endoscopic treatments
Endoscopic treatments are done using an endoscope (a thin tube-like instrument with a light and a magnifying glass) inserted into the esophagus. You may be offered endoscopic treatment to relieve symptoms of advanced esophageal cancer, such as difficulty swallowing. Some endoscopic treatments can also treat precancerous conditions and early cancers of the esophagus.
The following types of endoscopic treatment are used for esophageal cancer:
- endoscopic mucosal resection (EMR);
- endoscopic submucosal dissection (ESD);
- radiofrequency ablation (RFA);
- laser surgery;
- electrocoagulation or argon plasma coagulation;
- photodynamic therapy (PDT).
You can also use the endoscope to:
- put an endoprothesis in the esophagus to help keep it open;
- widen, or dilate, the esophagus where it is blocked;
- put a feeding tube in place.
If you cannot or do not want to be treated for cancer
You may want to consider care that aims to make you feel better without treating the cancer itself, perhaps because cancer treatments no longer work, or they are no longer likely to improve your condition, or cause them to work. secondary are difficult to tolerate. There may be other reasons why you cannot or do not want to be treated for cancer.
Talk to members of your healthcare team. They can help you choose advanced cancer care and treatment.
Monitoring
Follow-up after treatment is an important part of caring for people with cancer. You will need to have regular follow-up visits, especially during the first 2 years after treatment. These visits allow the healthcare team to monitor your progress and to know how you are recovering from treatment.
Clinical tests
Ask your doctor if there are clinical trials is available in your country for people with esophageal cancer. Clinical trials aim to find new methods of preventing, detecting and treating cancer.
Supportive care for esophageal cancer
Supportive care empowers people to overcome the physical, practical, emotional and spiritual barriers of esophageal cancer. It is an important component of the care of people with this disease. There are many programs and services that help meet the needs and improve the quality of life for these people and their loved ones, especially after treatment is over.
Recovering from esophageal cancer and adjusting to life after treatment is different for each person depending on the stage of the disease, the type of treatment received and many other factors. The end of cancer treatment can lead to mixed emotions. Even if treatment is complete, there may be other issues to work out, such as coping with long-term side effects. A person who has been treated for esophageal cancer may be concerned about the following.
Difficulty swallowing
Most people with esophageal cancer have difficulty swallowing (dysphagia). It can occur if:
the tumor blocks the esophagus;
food does not flow down the esophagus because the wave-like muscle contractions that occur in the esophagus (peristalsis) are different;
the esophagus is inflamed from radiation therapy.
You may also have difficulty swallowing due to an anastomotic stricture. Anastomotic narrowing occurs when the area where the end of the esophagus is attached to the end of the stomach has shrunk. This narrowing can be caused by scar tissue that forms after surgery or radiation therapy to the chest.
If you have difficulty swallowing, you may be offered endoscopic treatment among the following:
- esophageal dilation;
- placement of an esophageal stent graft;
- radiofrequency ablation (RFA);
- laser surgery;
- photodynamic therapy (PDT);
- electrocoagulation or argon plasma coagulation (not available in all treatment centers in Canada).
Nutritional disorders
Many people with esophageal cancer have nutritional problems. This could be because of the cancer itself, its treatments, or the side effects of treatments that can affect the digestive system and make it difficult to drink fluids and food.
Since esophageal cancer can affect your nutrition, the dietitian is a key member of your healthcare team. The dietitian can help make sure you are getting adequate nutrition during and after treatment.
Weightloss
Most people with esophageal cancer will lose a lot of weight. Significant weight loss is called cachexia.
Weight loss can occur if you have difficulty swallowing because of the tumor or treatments for esophageal cancer. Here are some side effects of treatment for esophageal cancer that can also cause weight loss:
- hunting syndrome (also called type II mucopolysaccharidosis (MPS II) – is a rare, life-threatening inherited disease. It represents a subgroup of lysosomal overload diseases and is extremely rare. It affects about 1 in 150,000 people worldwide);
- diarrhea;
- loss of appetite.
You may also lose weight if you have been diagnosed with advanced esophageal cancer. Advanced cancer causes changes in the body that affect its ability to use energy from food. The body therefore burns energy at a faster rate. This increased energy consumption, coupled with the fact that you eat less, causes weight loss.
It is important that you eat well and maintain your weight during and after treatment for esophageal cancer. Getting the right nutrition can help your body fight disease and cope with the effects of treatments.
To help manage the weight loss, your healthcare team may suggest the use of a feeding tube. The feeding tube is a thin, flexible tube that is inserted directly into the stomach or the upper part of the small intestine. Once the tube is in place, liquid nutritional supplements can be given to it.
People who have just been diagnosed with cancer of the esophagus because they have lost so much weight are often put on a feeding tube. You may also be fitted with a feeding tube before treatments such as chemoradiotherapy, as these may make swallowing and weight maintenance difficult.
If you have lost more than 10% of your body weight, your healthcare team may suggest parenteral nutrition (sometimes called total parenteral nutrition, or TPN). It delivers essential fluids and nutrients directly into the blood through an intravenous (IV) tube.
Tired
Many people with esophageal cancer experience fatigue. Fatigue can be caused by the cancer itself or its treatments. It may get worse if you have not been able to eat well because you had difficulty swallowing or if you have lost a lot of weight. People with advanced esophageal cancer can also experience a lot of fatigue.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, Mayo Clinic, American Cancer Society, National Cancer Institute (NCI) Cancer.gov, World Health Organization (WHO)
Photo credit: Wikimedia Commons