Carcinoma
Carcinoma is a type of cancer that develops from cells that make up the skin or the lining of organs in the body, such as the lungs, liver, or kidneys. It is a malignant tumor that grows and spreads rapidly, invading nearby tissues and organs and possibly spreading to other parts of the body.
Carcinomas are the most common type of cancer and can be classified into various subtypes based on their location and the type of cells they originate from. Treatment for carcinoma typically involves surgery, radiation therapy, and/or chemotherapy, depending on the stage and location of the cancer.
Carcinoma is one of the most common skin cancers. They are divided into basal cell carcinoma and squamous cell or squamous cell carcinoma.
What is the difference between carcinoma and melanoma?
Carcinoma and melanoma are very different. Carcinomas are the most frequent skin cancers, they are very frequent with age. They are also favored by the sun, rather chronic exposure. While some melanomas are favored by violent sunburn. Carcinomas are much less serious because they are usually removed and they rarely metastasize. Some can give some but they have to be big. Melanoma, even very small, can give metastases.
Two major types of very common carcinomas
Cutaneous carcinomas are the most common cancers in adults (30% of all cancers), and are also the most common skin cancers.
Two major types of cancer develop from epidermal cells, or keratinocytes, basal cell carcinomas and squamous cell carcinomas; they differ in behavior and prognosis. Adnexal carcinomas develop from skin appendages (hair, sebaceous or sweat glands) and are much rarer.
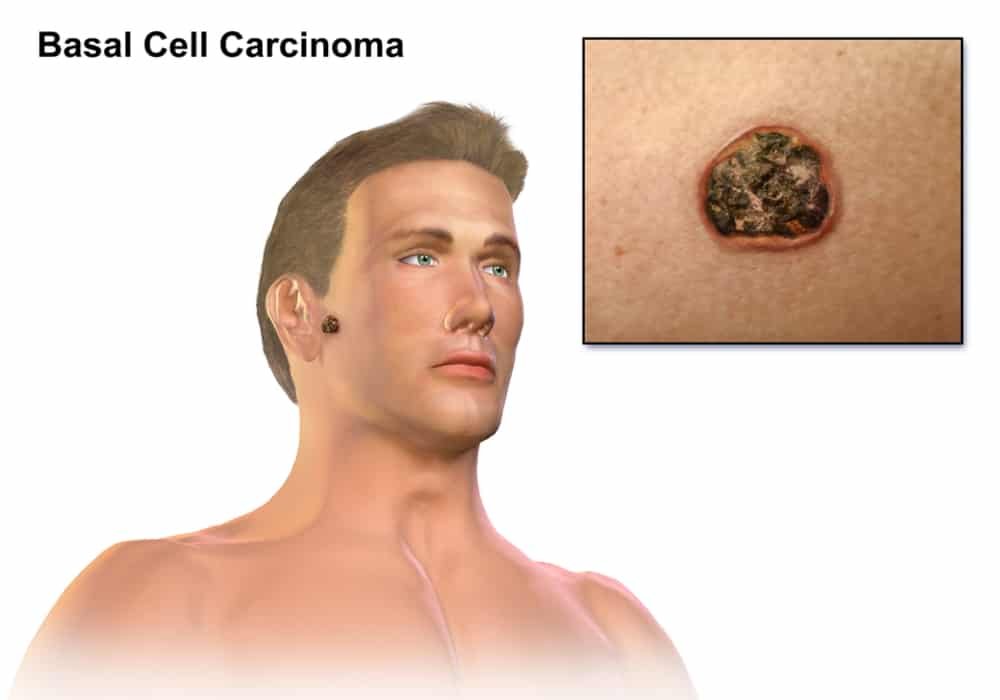
1. Basal cell carcinomas
Basal cell carcinomas are the most common skin cancers. It is estimated that there are about 70,000 cases each year for the entire French population.
There are several forms of basal cell carcinoma: superficial, nodular (the most common) and scleroderma with a higher risk of recurrence.
2. Squamous cell carcinomas
Squamous cell carcinomas are approximately 4 times less frequent.
There are also different forms of squamous cell carcinoma: superficial or carcinoma in situ also called Bowen’s disease, microinvasive or invasive of increasing severity.
Common elements
They are seen from the age of 50 and even rather later from the age of 60-65 for squamous cell carcinomas. Carcinomas affect men as well as women, with however a male predominance.
A very different risk for basal and squamous cell carcinomas
Basal cell carcinomas are tumors that have only local malignancy, they do not produce metastases, neither in the lymph nodes nor at a distance. If they are left to evolve for a long time, without treatment, they can develop in depth and invade the tissues which are under the skin, a muscle, a bone or even the organ which is under the cutaneous lesion. Nowadays, such developments have become very rare.
Squamous cell carcinoma is, on the contrary, a tumor capable of causing metastases in the lymph nodes or in distant organs (lungs in particular). Such dissemination is found in 2 to 5% of cases in the case of squamous cell carcinoma of the skin; this rate is higher, around 20%, when the squamous cell carcinoma has developed on a mucous membrane, for example on the lips or on the genitals.
Read also: Why Do Many People Get Cancer?
The causes
It’s important to note that in many cases, the exact cause of carcinoma is not known, and it is likely due to a combination of genetic and environmental factors. Early detection and treatment are important in improving the chances of a positive outcome.
The causes of carcinoma can vary depending on the type of cancer and the individual’s risk factors. Some common causes and risk factors associated with the development of carcinoma include:
Age
The risk of developing carcinoma increases with age.
Genetic mutations
Certain genetic mutations can increase the risk of developing some types of carcinoma, such as breast or colon cancer.
Environmental factors
Exposure to environmental toxins such as tobacco smoke, radiation, or certain chemicals can increase the risk of developing carcinoma.
Chronic inflammation
Long-term inflammation due to conditions such as ulcerative colitis, hepatitis B or C, or human papillomavirus (HPV) infection can increase the risk of developing certain types of carcinoma.
Weakened immune system
People with weakened immune systems, such as those with HIV/AIDS or those who have undergone an organ transplant, have an increased risk of developing some types of carcinoma.
Family history
People with a family history of certain types of carcinoma, such as breast, ovarian, or colon cancer, may have an increased risk of developing the same type of cancer.
The harmful effects of UV rays
People with the highest risk of being affected by this type of cancer have fair skin, light eyes and hair, have difficulty tanning and get sunburn easily.
The sun’s ultraviolet rays are capable of causing abnormalities in the keratinocyte nucleus, the cells of the epidermis and their DNA resulting in genetic mutations that can lead to cancerization of the cell. With aging, the body repairs these lesions less well, which explains why these cancers develop later.
Squamous cell carcinomas are more likely to be linked to chronic and prolonged exposure to the sun throughout their lives, which explains their greater frequency in a certain number of so-called exposed professions (farmers, road workers, sailors, instructors ports…).
Basal cell carcinomas, on the other hand, develop more readily in subjects who have had intermittent sun exposure and rather in childhood.
Given the importance of sun exposure in the appearance of the two types of skin carcinoma, it is clear that the populations at risk are fair-skinned populations and that sun protection is the best way to prevent them.
Tanning booths
Epidemiological studies, although discordant, show a tendency towards an increased risk of skin carcinoma in people using tanning booths early in life, and regularly thereafter, and the health authorities of very many countries strongly advise against tanning. use of these cabins. To limit its harmful effects, strict supervision (specific training for beauticians, ban on use before the age of 18, display of photosensitizing drugs in waiting rooms, etc.) has been in place for several years.
The viral track
For some years, it has appeared that certain infections linked to viruses of the human papillomavirus type (HPV for Human Papilloma Virus) could be the cause of squamous cell carcinoma, in particular at the level of the genital mucous membranes, but also of the skin, since 10 to 15 % of cutaneous squamous cell carcinomas could be related to a viral cause, particularly in immunocompromised patients. If a causal relationship were clearly established, we could hope for prevention through vaccination actions as effective as those which have been implemented for the prevention of cancers of the cervix, the main cause of which is infection with certain types of HPV.
The tobacco
Tobacco is an important factor favoring the appearance of squamous cell carcinoma of the lip. Its role in other types of skin carcinoma is not known.
Other causes
Other known causes of skin cancer include arsenic and coal tar, which promote both types of skin carcinoma. Radiotherapy which, at low doses, promotes the emergence of basal cell carcinomas after a delay of 20 to 25 years, can, at high doses, cause squamous cell carcinomas on radiodermatitis lesions.
You should also know that several chronic skin diseases, chronic skin wounds such as leg ulcers or even burn scars, can be the ground for the development of squamous cell carcinomas. As with other types of cancer, suffering from a chronic deficiency of the immune system due to disease (infection with the AIDS virus) or due to immunosuppressive treatment (in the case of transplant recipients), predisposes to development of squamous cell carcinomas. In these people, reinforced sun prevention and close dermatological monitoring are necessary.
Finally, actinic keratosis can turn into squamous cell carcinoma.
What exams?
The trained eye of the dermatologist, and a microscope
The diagnosis of cutaneous carcinoma is based on a thorough clinical examination aided by dermoscopy – a sort of medical magnifying glass – which makes it possible to make the diagnosis of carcinoma and sometimes of its histological subtype. The diagnosis will be confirmed by microscopic analysis.
supplemented by microscopic analysis of a sample of the tumor obtained by a skin biopsy.
Always think about it
The possibility of a cutaneous carcinoma-like tumor should be considered in the presence of any chronic skin lesion that has recently increased in size, is ulcerating or is bleeding slightly. This lesion can occur on previously healthy skin or in a place where the skin previously presented known abnormalities (radiodermatitis lesion, ulceration, burn scar, etc.).
Any lesion of this type calls for a dermatological consultation which will allow the clinical examination followed by the realization most frequently of a sample of the lesion by a skin biopsy (access to the chapter and the video on the skin biopsy) which will refute or will confirm the diagnosis.
The biopsy
The biopsy of the lesion performed by the dermatologist will be sent to a pathology laboratory where it will be prepared to be viewed under the microscope. This examination will thus make it possible to specify the nature of the tumour, basal or squamous cell carcinoma, and to specify its characteristics. There are indeed several types of basal cell and squamous cell carcinoma for which the treatment will not necessarily be identical. In general, the delay between the realization of the biopsy and the result is of the order of a few days. In the case of a small lesion, a biopsy which removes both the entire lesion and a sufficient area of healthy skin around this lesion constitutes both the procedure which confirms the diagnosis and which carries out the treatment.
The extension balance
In case of basal cell carcinoma, there is no particular assessment to be expected insofar as this type of carcinoma has a purely locoregional evolution. It is therefore only necessary to best assess the extension of the lesion on the surface and in depth to appreciate the importance of the surgical procedure to be performed.
In the case of squamous cell carcinoma, the draining lymph nodes should be analysed. The doctor therefore looks for possible damage to these lymph nodes both by carrying out a thorough clinical examination and with the help, if necessary, of ultrasound. Recourse to other examinations is only justified if there is clinical suspicion of involvement of one or the other remote organ.
Treatments
Primarily surgical treatment
It is recognized by all doctors specializing in the management of skin cancers that the standard treatment for basal and squamous cell carcinomas is surgery. The other methods of treatment are reserved for particular shapes or terrains. For the majority of carcinomas, surgery is effective in treating the tumor and its aesthetic and functional impact is extremely low.
Precise rules
The surgery of carcinomas follows well codified rules, one of the most important being the realization of an excision which must exceed the visible perimeter of the lesion which one removes. By removing an area of healthy tissue around the lesion, both on the surface and in depth (known as the excision margin), the surgeon helps to reduce the risk of recurrence from a few abnormal cells that would possibly have been located on the periphery of the lesion.
For basal cell carcinomas, this resection margin varies from 3 to 10 mm around the lesion, depending on the location as well as the particular clinical and histological type. For squamous cell carcinomas, the minimum resection margin is 5 mm, it is often 10 mm, or even more.
The surgical procedure is performed by a doctor familiar with skin cancers and skin surgery, a dermatologist or a plastic surgeon in particular.
Combine good oncological results
aesthetic AND
Depending on the size of the tumour, its location and the required excision margin, the piece of skin that will have to be removed can have very variable dimensions. It is therefore these 3 elements that will dictate the type of intervention.
Whenever functionally and aesthetically possible, the excision area benefits from a simple suture, resulting in the least visible scars; in this case, everything is settled in a week to 10 days.
If the simple suture is not possible, one can either leave the healing to take place alone with the help of “interface” healing fatty dressings which often make it possible to obtain a good quality scar, but requires two months to two months and half, either cover the operated area with a piece of skin that is moved from a neighboring area (technique known as skin flaps) or have recourse to a skin graft which is taken from the patient, with healing times of around 3 weeks for flaps to 2 months for grafts.
Clinical follow-up
Once the lesion has been removed, the patient must be followed regularly to identify a possible recurrence (every 6 months for the first year, then on an annual basis) or the possible appearance of another lesion, because it should be known that if the If you have already had a skin carcinoma, you have an increased risk of developing another.
It is also necessary to reinforce the sun protection.
A one or two-step intervention
In the simplest cases and for small lesions, in practice up to 5 mm, the treatment is done in a single stage, the biopsy being at the same time the surgical act of excision. For lesions that are more advanced or located in areas where it is aesthetically or functionally difficult to carry out a large intervention, the surgical act generally takes place after an initial small biopsy.
In cases where the sparing of the skin is important functionally or aesthetically, the surgical act is often done by passing as close as possible to the tumor, and it happens that the histological examination of the operative part indicates a margin of excision insufficient to guarantee a curative act, which requires a reoperation. It is possible to circumvent the difficulty in two ways:
By planning a two-stage surgery from the outset, i.e. removal of the lesion with the excision margins that seem appropriate and waiting for the results of the histological examination, before closing the area of intervention or , if necessary, remove additional skin to reach the healthy zone. Awaiting the result of the histological analysis, a fatty dressing is applied to the operated area to prevent infection and facilitate subsequent healing.
By using a so-called Mohs surgical technique (named after the surgeon who developed it) in which the edges of the area being removed are examined histologically “in real time”. This allows the surgeon to gradually complete his gesture until he is sure of being in the healthy zone on all sides of the excision. This surgery, which is technically difficult to perform, is underdeveloped in Europe due to limited indications. It is more practiced in the United States, partly for economic reasons favorable to surgeons who perform this type of intervention.
Given the high degree of sophistication of these two alternatives, they are in practice reserved for lesions which have a high risk of recurrence in the event of incomplete excision.
Other therapeutic possibilities
If surgical removal of the tumor is not possible for technical reasons or if it is contraindicated, it is possible to have recourse to radiotherapy which, however, gives less good results both in terms of control cancer and aesthetically. This technique is mainly used in very elderly inoperable subjects and in cases of tumors that are too large to be operated on without major sequelae.
For superficial tumors
For superficial tumors (superficial basal cell carcinomas, solar or actinic keratoses, Bowen’s disease or squamous cell carcinomas in situ), there are also two types of chemical treatments, imiquimod, and 5-fluorouracil and a treatment combining a chemical product with light: dynamic phototherapy. The use of these chemical treatments requires strict monitoring of patients, because the risk of recurrence is greater than with surgery.
For advanced or metastatic forms
For advanced or metastatic forms, targeted therapies have been developed for several years (= targeting the molecular anomaly at the origin of these tumours) which are more effective and better tolerated than conventional chemotherapy.
Finally, immunotherapy has recently become a therapeutic weapon for advanced forms of squamous cell carcinoma and is still being studied for basal cell carcinoma.
Dynamic phototherapy
There is also a method of treatment combining chemical and physical agents called dynamic phototherapy and consisting of applying a photosensitizing cream (or a precursor) to the lesion, then irradiating with an appropriate light source, most often a red light a few hours later. , allowing the destruction of cancerous cells. The results are very good on superficial carcinomas.
In general, chemical treatments and dynamic phototherapy are especially indicated in subjects who have recurrent superficial carcinomas. These treatments are alternatives to repetitive surgery, but require very strict monitoring because of the risk of recurrence.
Cryotherapy
Cryotherapy can also be proposed for superficial basal cell carcinomas. It has the advantage of being able to be done in consultation. In 80% of cases but can leave a depigmented scar.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, Cancer Center
Photo credit: BruceBlaus via Wikimedia Commons (CC BY-SA 4.0)