Brain Cancer
Brain cancer is a tumor lesion that develops in the skull at different levels. The symptoms are given by the localization, the morphological type and the evolution of the tumors.
Tests, such as magnetic resonance imaging (MRI), PET scan (positron emission tomoscintigraphy) and computed tomography (“CT scan”), can precisely locate the tumor. A biopsy (taking tumor tissue for analysis) is essential to determine the benign (non-cancerous) or malignant (cancerous) nature of the tumor.
Symptoms
When the tumor is small, it usually has no symptoms. But the bigger it gets, the more symptoms can occur.
Headaches (or headaches) are the most common symptom, regardless of the type of brain tumor. They often appear in the morning, sometimes accompanied by nausea and / or vomiting. They are due to the tumor mass compressing the area where it is located. As the tumor grows, it can limit the normal circulation of the fluid in which the brain bathes (cerebrospinal fluid). This results in high pressure in the skull (or intracranial hypertension). When the fluid accumulates significantly, it is called hydrocephalus.
Some patients also have convulsions or seizures, sometimes in the very early stages of the disease or later. They may or may not be accompanied by loss of consciousness. They are often the starting point for the diagnosis.
The patient may also present:
- speech, vision and hearing problems;
- dizziness or disturbed balance;
- memory impairment, learning or behavioral disturbances;
- partial paralysis.
These symptoms are not specific to brain tumors and may be due to other neurological conditions: diagnostic tests allow the doctor to rule them out before making the diagnosis of a brain tumor.
Read also: ATRT Atypical Teratoid Rhabdoid Tumor
Brain Cancer Stages
Grade and severity of the disease
Brain tumors are classified in increasing grades from I to IV according to increasing degree of aggressiveness and severity. This grade is determined from the data of the histological diagnosis, made by microscopic analysis of the biopsy sample. It guides future therapeutic choices. Slightly aggressive tumors are said to be benign (grade I) or low grade (grade II). Conversely, the most aggressive tumors are said to be anaplastic, malignant, cancerous or of high grade (corresponding to grade III or IV).
Chances of Surviving Brain Cancer
The outlook for a malignant brain tumour depends on things like where it is in the brain, its size, and what grade it is.
It can sometimes be cured if caught early on, but a brain tumour often comes back and sometimes it isn’t possible to remove it.
Brain cancers are rarely cancers that start in the brain. This is the case for only 2% of them. These are often metastases from other cancers, 25% of them leading to brain tumors. However, brain cancer is relatively common in children. The chances of survival depend largely on the type of brain cancer considered. Thus, people with a benign astrocytoma can in 90% of cases live 5 years on average while those with a glioblastoma (aggressive tumor) have an average survival of only 10 months. Very generally, the 5-year relative survival for brain cancer is 25%.
The prognosis for brain cancer is rather poor. This is even more true with terminal cancer. However, if the brain tumor is benign, the prognosis is good, even if the risks of sequelae are significant. Note that if the brain tumor is a metastasis from another cancer, the prognosis depends on that of the primary cancer.
Types of Brain Cancer
Benign and malignant tumors can be classified into different groups, depending on the type of cells from which they originate.
Benign tumors can be classified as follows:
- chordomas, the origin of which resides in embryonic cells of the spinal cord or the base of the cranial nerve;
- hemangioblastomas, which start in the blood vessels;
- meningiomas, starting in the membrane covering the brain;
- osteomas, in the bones of the skull;
- pinealomas, in the pineal gland;
- pituitary adenomas, in the pituitary gland;
- schwannomas, in the cells that surround the nerves.
- Some types of tumors, such as meningiomas (originating in the meninges, the lining around the brain) or germ cell tumors can be benign in some cases and malignant in others.
This article focuses on malignant (cancerous) brain tumors.
Brain cancers are relatively rare, but they are often fatal. The most common malignant brain tumors are gliomas, in which cells called neuroglial cells (cells that support nerve cells) become cancerous. Glioblastoma multiforme is the most common of all gliomas. Glioblastoma multiforme and anaplastic astrocytoma are rapidly growing gliomas. Oligodendroglioma, another type of glioma, also rare, occurs mostly in adults. Gliomas represent between 50% and 60% of all brain tumors (malignant and benign), children and adults combined.
Medulloblastoma, which arises from cells in the medulla oblongata at the base of the brain, is the most common type of brain tumor in children. It most often appears before puberty.
Finally, sarcoma and adenocarcinoma are two extremely rare types of brain tumor.

What are the names of brain tumors?
There are a large number of different brain tumors. Depending on their location, size and speed at which they grow, these tumors do not cause the same symptoms and do not have the same severity. Brain tumors are usually named after the cells from which they develop
• Glioma
These are the most well-known cancers, so called because the damaged cell is the glial cell which is found around neurons. The classification takes into account the degree of aggressiveness. There are several types, from I to IV, the first being the least aggressive.
• Glioblastoma
This is grade IV gliomas, it is the most aggressive and the most widespread. The treatments known today do not allow this disease to be cured. It only has means by chemotherapy and radiotherapy to lengthen it. life expectancy at one year, one and a half years.
• Meningioma
Meningioma affects cells in the meninges and can be localized around the brain and spinal cord. The most common form of meningioma is benign, and its prognosis favorable. There are also “malignant forms which require a surgical treatment and radiotherapy”.
• Medulloblastoma
It is a malignant lesion in the spinal cord and cerebellum. This tumor lesion appears mainly in children and adolescents. “As a symptom, this causes intracranial hypertension, walking and balance disorders. There are specific treatments and the possibility of curing depending on the stage of intervention”.
• Pituitary adenomas
It is a most often benign tumor that develops in the pituitary gland. “This gland, located behind the optic chiasm, in the pituitary fossa of the sphenoid bone, contains cells that produce hormones that regulate the activity of several organs. A pituitary adenoma can then create hormonal imbalances; adenoma the treatment will be medical or surgical. Pituitary adenomas are mostly benign lesions. If they are malignant, the prognosis is favorable if they are treated in time”.
• Cerebral lymphoma
Cerebral lymphoma particularly affects immunocompromised patients and people over the age of 60. “Its treatment is not practiced everywhere, because it requires close monitoring, heavy chemotherapy. Some patients can have a very long remission and there are many recurrences. Specialists are studying advanced treatments using stem cells. in order to improve the prognosis, which is still unfavorable for the moment “Survival is more important in young people”.
Diagnoses of Brain Cancer
As the symptoms are not specific, several examinations are necessary to make a diagnosis.
1. The clinical examination
The doctor questions the patient: he recapitulates with him his medical history, his family history and the clinical signs which could make suspect a tumor on the level of the brain. Then he performs a clinical examination. It checks intellectual functions, language, the quality of hearing, vision, touch, strength of limbs, coordination of gestures, reflexes, balance…
It emphasizes more particularly the functions affected by the symptoms felt by the patient.
2. Imagery
Two imaging tests are likely to be used:
in first intention, a scanner (or tomodensitometry – CT). It is effective in spotting 80% of tumors. The scanner makes it possible to confirm or not the presence of a tumor and, if necessary, to specify its position and size. The CT scan provides X-ray images of the brain. Before the exam, an iodinated contrast medium is injected into a patient’s vein to make the tumor easier to visualize. The patient is then lying on a table located at the heart of a large ring that emits the radiation. The exam lasts about twenty minutes;
Magnetic Resonance Imaging (MRI) can identify tumors that would not have been seen on the CT images. This examination is more sensitive and tends to gradually replace the first-line scanner. The images obtained also have the advantage of better describing the tumor – exact location, size, possible extension to other structures of the nervous system (meninges, spinal cord, etc.) – and of collecting data that will facilitate local treatments used subsequently ( surgery and / or radiotherapy).
In practice, the process of MRI is similar to that of a scanner, but it uses an electromagnetic field instead of radiation.
Lumbar puncture
A lumbar puncture must sometimes be performed to clarify the diagnosis. It involves inserting a fine needle into the bottom of the spine to take a sample of the cerebrospinal fluid, in which both the spinal cord and the brain structures are bathed. The sample is then analyzed for possible tumor cells.
3. Biopsy
The biopsy is the gesture that confirms the diagnosis with certainty. This involves taking a sample of tissue from the tumor. It can be performed using two techniques: by stereotaxis or by craniotomy.
Stereotactic biopsy is a technique allowing a sample to be taken with millimeter precision. The sample area is identified by imagery and its coordinates are defined in a three-dimensional geometric space through the use of a stereotaxic frame. At the start of the examination, a frame is attached to the skull under local anesthesia. The patient is then subjected to imaging examination, by CT scan or MRI. Once the tumor has been located, the coordinates established in the frame of reference of the stereotaxic framework are used to indicate the site and angle of introduction of the needle as well as its depth of penetration to precisely reach the tumor. The surgeon makes an incision of a few millimeters in the skull (trepanation) in order to insert the needle and take the sample from the tumor. The sample is then analyzed by microscopy.
Biopsy after craniotomy or “open” is considered when the tumor is superficial and easily accessible and when it is located in a non-functional area of the brain. The sample taken is then analyzed by microscopy. It is also used when the probability that the lesion is cancerous is high. In this case, the surgeon immediately removes all of the tumor, which will then be analyzed by microscopy.
In practice, the craniotomy consists of opening the cranial box under general anesthesia. The neurosurgeon cuts out part of the skull bone and then cuts through the meninges to access the tumor. After having partially or completely removed the tumor, the bone is put back in place and fixed. This operation requires one week of hospitalization.
Regardless of the type of biopsy, the results of the analysis of the collected sample provide precise information on the nature of the tumor. The diagnosis can be made and doctors make a treatment plan that also takes into account the age and general condition of the patient.
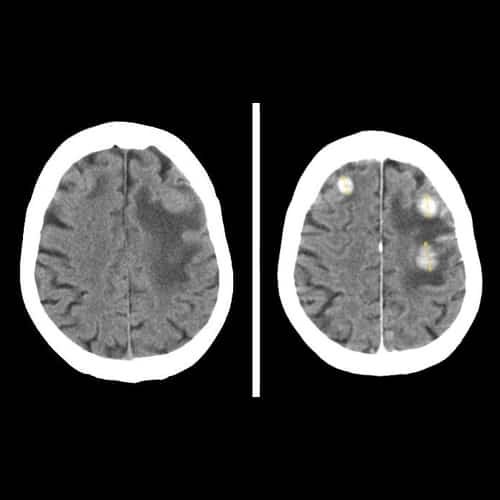
Photo credit: Wikimedia Commons
Treatments
1. Surgery
Surgery is the standard treatment for brain tumors, whether benign or malignant. It is considered in cases where the location of the tumor allows it.
Surgery can also be used for decompressive purposes: the cranial box being inextensible, an increase in the volume of its contents linked to the presence of tumors can generate too much intracranial pressure and ultimately plunge the patient into a coma. The purpose of surgery is to remove enough tumor tissue to limit this risk of hyperpressure.
Surgery is not always recommended:
in the case of benign tumors which have weak growth and / or which cause few symptoms and / or which have a complex localization, regular monitoring is preferred.
Surgery will only be offered if symptoms appear and / or if imaging tests reveal tumor development;
in the case of infiltrating tumors whose boundaries are not clearly identifiable, surgery can be dangerous and unnecessary;
in the case of tumors located in areas that are difficult to access and / or extensive in deep brain tissue, the procedure may be risky. Treatment by radiotherapy and / or chemotherapy is then preferred. Surgery can sometimes become possible later. This is called radiotherapy and / or neo-adjuvant chemotherapy, that is to say carried out before the surgery.
In practice
Surgical removal is done by craniotomy, under general anesthesia: the patient’s hair is first shaved approximately 1 cm wide on either side of the area to be incised. The skin of the skull is also incised and folded back to reveal the bone next to the tumor. The skull then the meninges are open a few centimeters.
The surgeon can then intervene: he partially or totally removes the tumor tissue. The meninges are then stitched up, the bone rested and reattached to the rest of the skull with wires or metal ties. Finally the skin is sutured for healing.
To make the surgical removal as precise and less invasive as possible, several technical aids exist:
Neuronavigation
Neuronavigation is a system that combines computing and medical imaging. It makes it possible to locate and access the tumor with great precision. A 3D image of the brain is first reconstructed by computer from images obtained by MRI and / or by scanner. Thanks to this image, the neurosurgeon can determine the best approach technique and the most suitable surgical procedures and the least risky in terms of sequelae. It also allows him to train before the operation through simulations of the operation.
During the procedure, a camera system matches the images of the brain as recorded live with those, in 3D, which have been reconstructed previously. The surgeon can then direct his surgical instruments to match their position to that which had been planned. The juxtaposition of images can be viewed on a monitor screen or, if the operation is performed using a microscope, directly in the eyepieces. The ablation is thus more precise and the risks associated with the intervention are better controlled, especially when the tumor is small and / or located in a region of the brain at risk of sequelae.
Cortical stimulation
When the tumor is close to very well defined areas of the brain that control essential functions, the surgeon can stimulate these during the procedure. With a stylus, he delivers small pulses to neighboring areas of the tumor and observes the functions they control: he can thus identify more precisely those associated with important functions and that he must avoid during the intervention. . Depending on the case, functional areas of the brain, such as motor skills, can be stimulated in a sleeping patient. Others, on the other hand, ask that the patient be awake (the language area for example). In this case, surgery should be performed on the awake patient, then placed under locoregional anesthesia. The surgeon can thus remove a maximum of abnormal tissue while limiting the removal of normal areas necessary for the essential functions of the patient. Operations on an awake patient thus limit the risk of sequelae.
Follow-up to the operation
In the short term, the patient who has had head surgery may experience headaches and local pain. These symptoms can be relieved with suitable medication.
After the operation, the operated area may also bleed and the patient may present with edema of the brain, face and eyes (related to the shrinking of the skin of the skull); these edemas usually go away after a week, during which time specific treatment may be prescribed.
Very rarely, a local bacterial infection can also develop in the operated area. In this case, antibiotic treatment is prescribed.
The skin usually heals after a week. The bones of the skull gradually reseal over a few days to a few weeks. The hair grows back normally and completely masks the scar after a few weeks.
In most cases, the symptoms that were due to the tumor resolve within a few days or months. However, some may persist partially or totally, temporarily or permanently. It is often impossible to predict this development.
Also, although it is usually uncomplicated, the brain surgery can sometimes have sequelae. This organ is indeed particularly delicate to operate and its relatively limited recovery capacities. The neurosurgeon therefore informs the patient of the potential consequences of the proposed operation.
If sequelae exist following the operation, treatment can be put in place to relieve or reduce them.
2. Radiotherapy
Radiation therapy is one of the most widely used treatments in the management of primary brain tumors. It uses ionizing rays whose high energy kills cancer cells.
This radiation is focused on the tumor in order to concentrate its energy on the tumor cells and to limit its impact on neighboring healthy tissues. However, the healthy cells surrounding the tumor can be affected and their damage can cause transient side effects. Radiation therapy is often used after surgery, alone or in combination with chemotherapy. It can also be considered without surgery, alone or in combination with chemotherapy.
In any case, its implementation includes several stages, all of which are called the treatment plan. First, a preparatory CT or MRI is scheduled. This examination allows the radiotherapist to define very precisely how the radiotherapy device should be used and positioned during treatment sessions and to calculate the total dose and the number of sessions to be planned (the irradiation schedule) to destroy the tumor while preserving the healthy areas as well as possible.
Between this preparatory examination and the various radiotherapy sessions, the patient’s position must be scrupulously identical. For this, a marking point (tattoo or marker) can serve as a reference point. A compression mask, once placed on the head, helps the patient to be perfectly still during the different sessions.
There are different radiotherapy techniques used to deliver the radiation as precisely as possible to the tumor tissue:
three-dimensional conformational radiotherapy is the most widely used technique today in the treatment of brain tumors. It optimizes the dose to be administered by precisely calculating the way to position the beam of rays on the volume to be treated. It uses for this the 3D images which were obtained by scanner and / or MRI;
conformational radiotherapy with modulation of intensity is based on the same principle as three-dimensional conformational radiotherapy. The difference lies in the ability of the device to modulate the intensity of the beam delivered during the same session depending on the treated area of the tumor;
Radiotherapy under stereotaxic conditions is a recent method which makes it possible above all to treat small, well-defined tumors, especially when they are difficult to access by surgery. It uses converging beams of rays that irradiate the tumor with millimeter precision. It can thus concentrate a sufficient dose on the tumor mass in order to destroy it. When a single session is sufficient, we also speak of “radiosurgery”, irradiation replacing surgery. For certain tumors, this treatment is carried out in several sessions: we speak of radiotherapy in hypofractionated stereotaxic conditions. To ensure the accuracy of the radiation, the patient’s head is held in a stereotaxic frame.
In practice
The most widely used irradiation regimen today is called the “classic fractionation regimen”: it includes a daily session every day of the week except weekends and holidays. The number of weeks of treatment depends on the total dose to be delivered, which depends on the type of brain tumor. The daily duration of a typical session is 10 to 15 minutes. The irradiation itself lasts only a few minutes, most of the session being reserved for checking the treatment position. More rarely, a single radiotherapy session or a few sessions (from 3 to 10) spread over one or two weeks may be offered for small relapsing tumors, for example.
Side effects
Some side effects can occur with brain irradiation. The dose of radiation, the radiotherapy technique used, and the location of the tumor influence the occurrence of these effects.
Brain edema may occur within a few weeks of starting treatment. It doesn’t always cause symptoms, but when it does, headache, nausea and / or fatigue can occur. Sometimes radiation therapy worsens pre-existing symptoms related to the tumor. Corticosteroid therapy is prescribed to resolve the edema and its related symptoms.
The second most common side effect after irradiation is alopecia (hair loss). It is located at the level of the areas on which the rays are oriented. It can occur after 2 to 3 weeks. Its importance depends on the dose delivered by each beam. It may or may not be definitive, depending on the dose delivered and the area irradiated.
Brain radiotherapy can cause other side effects which can be transient or persist in the long term: epileptic seizures, skin reaction, drowsiness, disturbance of cognitive functions … Their occurrence and intensity depends on the type of tumor, its location and patient profile. Most of the time, treatments can be offered to relieve or reduce these effects.
3. Chemotherapy
Chemotherapy is the administration of drugs that destroy tumor cells. It is sometimes the only possible treatment option, especially when the tumor is inoperable.
It can be used alone or in combination with radiotherapy, before or after the operation. Before the operation, it makes it possible to reduce the tumor volume to facilitate the surgical procedure. After the operation, its role is to destroy residual cancer cells.
Chemotherapy can also be used at the same time as radiotherapy (this is called concomitant radiochemotherapy). It then has the advantage of making the tumor more sensitive to the effect of the rays. In practice, the use of chemotherapy in the treatment of brain tumors is limited by the ability of the drugs to reach the brain. Indeed, only certain molecules manage to cross the blood-brain barrier.
Course of chemotherapy
As a general rule, chemotherapy protocols last several weeks: depending on the nature and stage of the tumor, one or more drugs are administered in precise doses which sometimes vary over time. The most frequently used molecules are temozolomide, carmustine, fotemustine, procarbazine, platinum, vincristine. Often several cycles of treatment are necessary, spaced a few days or weeks apart.
Chemotherapy is administered by injection or by mouth. To avoid multiple punctures in the patient’s veins, a catheter can be placed under the skin while the entire protocol is being carried out. Depending on the case, the team will use a catheter whose end, implanted under the skin, is located at the level of the collarbone, or a small reservoir (implantable chamber).
Side effects
The side effects induced by chemotherapy depend directly on the nature of the drug used: in the case of the treatment of brain tumors, it is mainly a transient decrease in the number of red blood cells, white blood cells or platelets in the blood, which can respectively induce anemia (fatigue), risk of infection or bleeding. In other cases, the patient may suffer from digestive problems (diarrhea, vomiting) or hair loss which lasts for the duration of the treatment. Most often, these side effects can be reduced with treatment.
4. Carmustine implants (glial wafers)
A new way of giving chemotherapy for some high-grade tumours, where implants are inserted into the brain. During brain surgery to remove most or all of a tumour, up to 8 implants are inserted into the space where the tumour was. They then gradually release carmustine into this area over 2–3 weeks. Temozolomide (also known as Temodal) is given as tablets to treat the tumour, first with radiotherapy and then on its own.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, The Johns Hopkins University, Cancer Center, American Society of Clinical Oncology (ASCO), MediciNet, United Kingdom National Health Service (NHS), National Cancer Institute, Yale University
Photo credit (for illustration): Pixabay