List of Heart Diseases (cardiovascular diseases)
Cardiovascular diseases or heart diseases include pathologies that affect the heart and all of the blood vessels, such as atherosclerosis, heart rhythm disturbances, arterial hypertension, myocardial infarction, heart failure or even stroke. . Heart diseases are caused by dysfunctions of the heart or blood vessels, they are particularly favored by smoking and an unbalanced diet and are responsible for a very large proportion of deaths in the population. Their diagnosis, most often carried out by a cardiologist, involves various medical examinations (electrocardiogram, MRI, ultrasound…).
What are the risk factors?
The main risk factors for heart disease and stroke are poor diet, lack of physical activity, smoking and harmful use of alcohol.
The effects of behavioral risk factors can cause people to have high blood pressure, high blood sugar, hyperlipidemia, overweight and obesity. These “intermediate risk factors” can be assessed in primary health care settings and are indicative of an increased risk of heart attack, stroke, heart failure and other complications.
Quitting smoking, reducing salt intake in your diet, consuming fruits and vegetables, exercising regularly and avoiding the harmful use of alcohol have been found to reduce the risk of heart diseases. In addition, drug treatment for diabetes, hypertension and hyperlipidemia may be necessary to decrease heart diseases risk and prevent heart attacks and strokes. Health policies, which create the conditions for making good health choices both affordable and possible, are essential to encourage people to adopt and stick to healthy behavior.
Read also: Cholesterol (excess) | symptoms, causes, treatments, levels, foods, warning, dietary supplements
There are also a number of underlying determinants of heart diseases. They come from the main social, economic and cultural developments – globalization, urbanization and the aging of the population. Other determinants of heart diseases are poverty, stress and hereditary factors.
September 29: World Heart Day
Many cardiovascular diseases can be prevented. Everyone can act for better lifestyle habits: stop smoking, adopt a balanced diet, maintain regular physical activity, reduce sedentary behavior, reduce alcohol consumption, act on stress, reduce overweight. With health professionals, it is a question of evaluating the risk and reducing clinical factors such as arterial hypertension, type 2 diabetes, hypercholesterolemia, obesity or certain heart rhythm disorders.
The improvement of lifestyle habits, and drug treatments if necessary, complement each other to reduce an often multiple risk.
Hypertension
- Hypertension – elevated blood pressure above “normal.” Long term high blood pressure is a major risk factor for coronary artery disease, stroke, heart failure, peripheral vascular disease, vision loss, and chronic kidney disease. Lowering blood pressure is key for preventing these diseases.
- Types of hypertension
- Essential hypertension – Hypertension with no known cause, which is about 90–95% of people with hypertension. Often thought to be due to lifestyle. Management is through medications and blood pressure that does not respond is a red flag that it may be secondary hypertension. Due to the widespread nature of hypertension, cardiologists will end up managing or recommending treatments for essential hypertension.
- Secondary hypertension – Most causes of secondary hypertension are from kidney and endocrine disorders. Cardiovascular causes of hypertension include coarctation of aorta, atherosclerosis, and aortic stenosis.
- Complications of hypertension
- Hypertrophic cardiomyopathy – Increased pressure results in hypertrophy of the myocardium, particularly left ventricular hypertrophy. Pulmonary hypertension — which is separate from “hypertension” described above — can result in right ventricular hypertrophy.
- Hypertensive crisis – Generally considered to be a systolic blood pressure over 180. If there is no organ dysfunction it is called a hypertensive urgency, but if there is (e.g., confusion, breathlessness) then it is called hypertensive emergency.
- Pre-eclampsia (PreE) / Eclampsia – PreE is a disease of pregnancy that results in hypertension and proteinuria. PreE has negative consequences for both the mother and fetus/baby. Progression to eclampsia involves seizures. Currently, the only definitive treatment is delivery of the fetus.
- Hemorrhagic stroke – Infarction of the brain due to internal bleeding from Charcot–Bouchard aneurysms.
- Hypertensive encephalopathy, hypertensive nephropathy, hypertensive retinopathy – Damage to organs from chronic hypertension.
- Types of hypertension
Cardiac arrhythmias
- Cardiac arrhythmias – conditions in which the heartbeat is irregular, too fast, or too slow. Many types of arrhythmia have no symptoms. When symptoms are present these may include palpitations or feeling a pause between heartbeats. More seriously there may be lightheadedness, passing out, shortness of breath, or chest pain. While most types of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in cardiac arrest.
- Atrial fibrillation (afib or AF) – Fibrillation of the atria is fairly common and more common with increased age and overall disease of the heart. If the ventricular rate exceeds 100 then the afib is further classified as “afib with RVR” meaning rapid ventricular response.
- Atrial flutter (AFL) – A re-entrant tachycardia greater than 240 beats per minute and produces a characteristic saw-tooth pattern on ECG. It often degenerates to atrial fibrillation.
- Heart block – A decrease in the ability of the conduction system to transmit action pulses in the orderly manner. Blockage of the signal at different areas results in different types of heart block (e.g., first-degree AV block, left bundle branch block).
- Long QT syndrome – Lengthening of the QT interval can result in arrhythmias and sudden cardiac death. Specifically, it can lead to torsades de pointes than can then lead to ventricular fibrillation. It can be an inherited disorder or be acquired. Certain medications are associated with lengthening of the QT interval — drug-induced QT prolongation — and an EKG may be warranted before starting the medication to ensure a normal QT interval, but this practice is debated.
- Premature atrial contractions (PACs or APCs) – Normal beats originate in the SA node and extra beats originating from the atria are called PACs. They can be found in normal hearts and be asymptomatic; symptomatic PACs can be treated with beta blockers. PACs, like PVCs, can pair up with normal beats in a pattern called bigeminy.
- Premature ventricular contractions (PVCs) – Normal beats are conducted through the AV node to the ventricles resulting in a narrow QRS complex. With PVCs, the extra beat originates within the ventricles and results in a wide QRS complex. Like PACs, they can be found in healthy hearts but are more likely to be found in bigeminy than PACs.
- Sick sinus syndrome, Bradycardia-tachycardia syndrome (BTS) – Disease of the SA node that results in irregular changes in heart rate and in the case of BTS the arrhythmia alternates between bradycardia and tachycardia.
- Supraventricular tachycardia (SVT) – A collection of tachycardia rhythms that originate before the ventricles and include the SA node, atria, and AV node. It is a broad, encomparsing term that includes other rhythms in this list (e.g., afib with RVR) and others.
- Torsades de pointes – A polymorphic arrhythmia that can be syptomatic and tends to resolve to a normal sinus rhythm. However, there is a concern
- Ventricular fibrillation (vfib) – Fibrillation of the ventricles is a life-threatening arrhythmia and should be treated by defibrillation and is a medical emergency. Vfib results from uncoordinated contraction of the ventricles and defibrillation acts as a ‘reset’ to synchronize contraction (i.e., a normal rhythm).
- Ventricular tachycardia (vtach) – Tachycardia that originates from within the ventricles. Typically, “vtach” implies monomorphology but it can be an umbrella term for both monomorphic and polymorphic (i.e., torsade de pointes). To classify a ventricular rhythm as vtach, at least 3 beats in a row must originate from the ventricles and have a rate over 100. If it lasts longer than 30 seconds, it can additionally be labelled as a sustained vtach.
Coronary circulation disorders
- Coronary circulation disorders
- Atherosclerosis – Atherosclerosis is the condition in which an artery wall thickens as the result of a build-up of fatty materials (e.g., cholesterol) and white blood cells (“foam cells”). Atherosclerosis of a coronary artery leads to coronary artery disease (CAD). Atherosclerosis is a broad term referring to loss of elasticity of arteries and more specific terms exist — arteriosclerosis and arteriolosclerosis — to narrow which arteries are diseased and can easily be confused due to similar spelling. Overall, atherosclerosis tends to affect the arteries of highest pressure: aorta, coronary, renal, femoral, cerebral, and carotid.
- Coronary artery disease (CAD) – Coronary artery disease is a general term for any reduction in coronary circulation. One such cause is atherosclerosis. CAD can lead to ischemia (angina pectoris) or infarction (myocardial infarction). Treatment of CAD includes angioplasty, stenting, and coronary artery bypass surgery (CABG).
- Acute coronary syndrome (ACS) – ACS is a medical emergency and is a broad term encompassing many acute myocardial infarction symptoms. As a syndrome, it consists of a constellation of symptoms and can have many causes. The top three causes of ACS are ST elevation myocardial infarction (STEMI, 30%), non ST elevation myocardial infarction (NSTEMI, 25%), or unstable angina (38%). The first two are myocardial infarctions which are more commonly known as “heart attacks.”
- Angina pectoris – Angina pectoris literally means “chest pain” that refers to pain caused by ischemia of the heart. The main cause of angina is coronary artery disease, but can result from other non-atherosclerotic causes such as anemia and heart failure. Stable angina results if the angina resolves with rest or nitroglycerin, but can progress to unstable angina which is a form of acute coronary syndrome.
- Myocardial infarction (a.k.a. heart attack) – A myocardial infarction is the death of a part of the heart which is typically caused by a blockage of the coronary circulation but can be caused by other insufficiency such as cardiogenic shock.
- Restenosis – Recurrence of stenosis after being treated (e.g., stenting).
Cardiac arrest
- Cardiac arrest – cessation of normal systemic circulation due to failure in proper contraction of the heart. There are several conditions that can cause cardiac arrest. Treatment of cardiac arrest includes cardiopulmonary resuscitation (CPR), defibrillation, and advanced cardiac life support (ACLS), and treatment of the underlying cause of arrest.
- Asystole (“flatline”) – Asystole refers to the absence of electrical activity of the heart and is sometimes referred to as a “flatline” because the electrocardiogram shows a solid line due to the absence of electrical activity. This flatline is commonly used in television and movies to signal death. There are numerous causes of asystole that may be reversible if determined quickly enough, however, survival is very unlikely (~2% if not in a hospital). In contrast, asystole is desired and induced during cardiopulmonary bypass through a cardioplegia solution containing very high amounts of potassium. One additional example is the use of high potassium in lethal injection that results in asystole, cardiac arrest, and then death.
- Pulseless electrical activity (PEA) – Pulseless electrical activity is when the electrocardiogram shows a rhythm that should produce a pulse but it does not. PEA is commonly caused by the 6 H’s and 6 T’s (see PEA article) and results in decreased cardiac output and insufficient oxygen delivery to the body.
- Pulseless ventricular tachycardia – Pulseless ventricular tachycardia (VT) Is one classification of VT such that no pulse is felt because of an ineffective cardiac output which causes cardiac arrest, which also results in insufficient oxygen delivery to the body.
- Sudden cardiac death (SCD) – concept of natural death rather than a specific medical condition. There are several causes of sudden cardiac death and it is distinct from cardiac arrest. The leading cause of SCD in young athletes is hypertrophic cardiomyopathy but can also result from commotio cordis that is often sustained during athletic activity.
- Ventricular fibrillation – Ventricular fibrillation is fibrillation of the ventricles of the heart. Rhythmic contraction is necessary for efficient movement of blood, and fibrillation disrupts this rhythm sufficiently to cause cardiac arrest.
Disorders of the myocardium
- Disorders of the myocardium
- Cardiomyopathy – Cardiomyopathy is a deterioration of the myocardium. Several classifications have been used to categorize cardiomyopathies with the most common being primary vs. secondary, and dilated vs. restrictive vs. hypertrophic (presented below).
- Ischemic cardiomyopathy – Cardiomyopathy causing ischemia of the heart due to coronary artery disease.
- Nonischemic cardiomyopathy – Cardiomyopathy caused by something other than ischemia.
- Amyloid cardiomyopathy – Cardiomyopathy caused by amyloidosis.
- Hypertrophic cardiomyopathy (HCM) – Cardiomyopathy caused by hypertrophy of the heart and is the leading cause of sudden cardiac death in young adults.
- Hypertrophic obstructive cardiomyopathy (HOCM) (Idiopathic hypertrophic subaortic stenosis (IHSS)) :
- Dilated cardiomyopathy (DCM) – Cardiomyopathy caused by dilation of the heart, typically caused by “drugs and bugs.” It is the most common form of non-ischemic cardiomyopathy and the dilitation of the heart results in larger chamber volumes & thinner myocardial walls, both of which decrease the ability to pump. Specific kinds of dilated cardiomyopathy are listed below, and other causes include Chagas disease, chemotherapeutic agents (e.g., doxorubicin), tuberculosis, and pregnancy.
- Alcoholic cardiomyopathy – A type of dilated cardiomyopathy caused by chronic abuse of alcohol and results from direct toxicity of ethanol on the myocardium.
- Tachycardia induced cardiomyopathy – A type of dilated cardiomyopathy caused by chronic tachycardia. A common arrhythmia that can lead to this form of cardiomyopathy is the common atrial fibrillation.
- Takotsubo cardiomyopathy (Transient apical ballooning, stress-induced cardiomyopathy) – A type of dilated cardiomyopathy caused by a sudden temporary weakening of the myocardium, which can include emotional stress (i.e. broken-heart syndrome). It presents as sudden heart failure with ECG changes similarly found in myocardial infarction and typically is found in post-menopausal women.
- Arrhythmogenic right ventricular dysplasia (Arrhythmogenic right ventricular cardiomyopathy) – Cardiomyopathy caused by a genetic mutation of the desmosomes that connect myocytes.
- Restrictive cardiomyopathy (RCM) – Cardiomyopathy caused by excessive rigidity of the heart that prevents effective contraction and pumping. In comparison to DCM, RCM is often secondarily caused by other diseases such as amyloidosis, scleroderma, hemachromatosis (iron overload) and eosinophilic granulomatosis with polyangiitis. As such, the treatment for RCM is to treat the disease causing the RCM.
- Heart failure – Heart failure is failure of the heart to produce sufficient blood flow to meet metabolic demands of the body, or to do so at higher filling pressures. The hallmark signs of heart failure include shortness of breath (especially on exertion, at night, or while lying down) and leg swelling. Chest pain is rarely a feature of heart failure, which would point a diagnosis more toward angina pectoris or myocardial infarction. Perhaps confusingly, heart failure can be caused by coronary artery disease (CAD) and myocardial infarction (MI) that result in a deficiency in pumping that then leads to heart failure. Treatment of heart failure, like most secondary disorders, depends upon treatment of the primary cause which includes CAD & MI but also valvular problems like aortic stenosis and hypertension.
- Cor pulmonale – Untreated cor pulmonale can cause right heart failure from chronic pulmonary hypertrophy.
- Ventricular hypertrophy – Hypertrophy of the ventricle. Thickening of the myocardium (i.e., hypertrophy) can be physiological (a normal response) or pathological. An example of physiological hypertrophy is the result of significant athletic training (athletic heart syndrome).
- Left ventricular hypertrophy (LVH) – Hypertrophy of the left ventricle is more common than in the right and typically due to increased afterload on the heart such as from hypertension and aortic stenosis, but also from long standing mitral valve regurgitation. It can be diagnosed by echocardiography or ECG.
- Right ventricular hypertrophy (RVH) – Hypertrophy of the right ventricle and, it too, can be physiological from athletic training. Other causes include pulmonary hypertension and COPD as well as several congenital heart defects like ventricular septal defect, Tetralogy of Fallot and hypoplastic left heart syndrome.
- Heart cancer – Cancer of the heart is very rare and those cancers tend to be benign.
- Myxoma – Most common tumor of the heart. It is a benign tumor most commonly found in the left atrium and can be associated with Carney syndrome.
- Myocardial rupture and ventricular aneurysm – Rupture is a gross structural failure of the heart. Commonly a result of myocardial infarction that weakens the wall sufficiently to result in frank rupture and is typically seen 7–10 days after infarction. If not significant enough, the wall can develop into a ventricular aneurysm.
- Myocarditis – Infection and inflammation of the myocardium is myocarditis. Most causes are infectious (parvovirus B19, Lyme disease, Chagas disease), toxic (ethanol, anthracyclines, clozapine), or immunologic (systemic lupus erythematosus, sarcoidosis, and some of the vasculitides (see below)). Definitive diagnosis requires a biopsy.
- Uhl anomaly – A congenital heart defect in which the right ventricular myocardium is too thin or absent. It is a very rare disorder.
- Cardiomyopathy – Cardiomyopathy is a deterioration of the myocardium. Several classifications have been used to categorize cardiomyopathies with the most common being primary vs. secondary, and dilated vs. restrictive vs. hypertrophic (presented below).
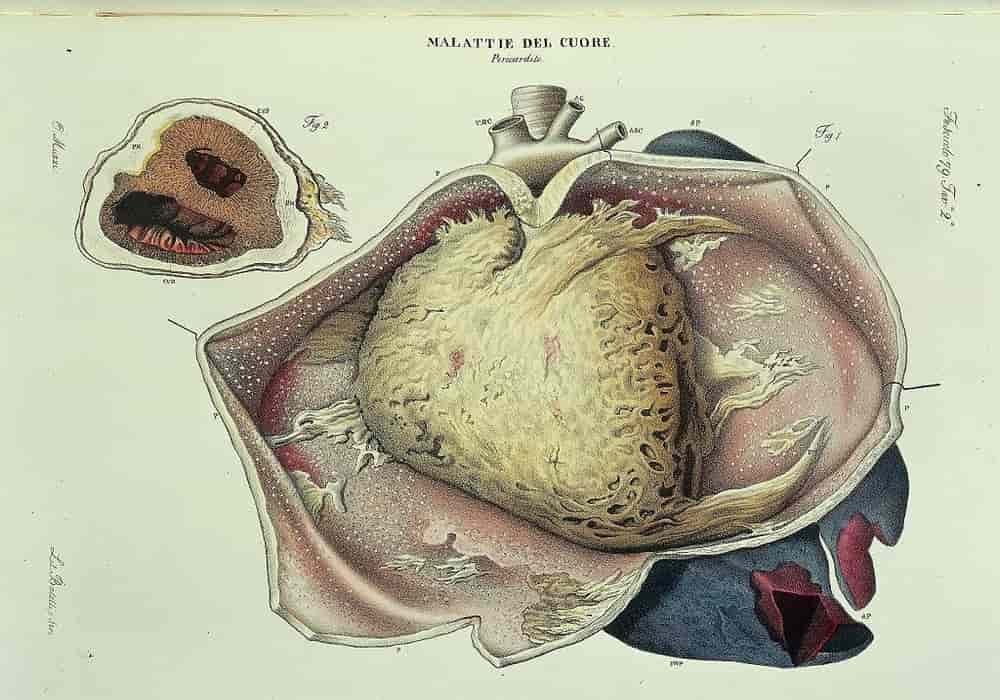
Disorders of the pericardium
- Disorders of the pericardium
- Pericarditis – Inflammation of the pericardium that is typically idiopathic or infectious in nature (the membrane covering the heart). This inflammation is accompanied by swelling at the level of this membrane, in particular due to an excess of fluid circulating between the pericardium and the heart. The main symptoms of pericarditis are pain in the chest. These pains can occur suddenly, sharply and severely. The pain is usually worse at night when lying down and less when sitting. Treatment of viral & idiopathic pericarditis is NSAIDs or aspirin.
- Constrictive pericarditis – Pericarditis that constricts the expansion of the heart and inhibits heart function. Causes include infections (tuberculosis, fungus, parasites) and surgery. Definitive surgery is a pericardiectomy.
- Dressler syndrome – A form of pericarditis that develops 2–3 weeks after myocardial infarction and is accompanied by fever, pleuritic chest pain, and symptoms of pericarditis.
- Constrictive pericarditis – Pericarditis that constricts the expansion of the heart and inhibits heart function. Causes include infections (tuberculosis, fungus, parasites) and surgery. Definitive surgery is a pericardiectomy.
- Pericardial effusion – The serous pericardium normally contains fluid that reduces friction, but an abnormal accumulation of fluid in the pericardium is called a pericardial effusion. The list of causes is lengthy but includes pericarditis, rheumatic diseases (e.g., systemic lupus erythematosus), trauma, and blood from myocardial rupture. If an effusion worsens then the fluid can inhibit heart function and symptoms of cardiac tamponade appear. Treatment includes pericardiocentesis to drain the fluid, if necessary, and treatment of the underlying cause.
- Pericardial tamponade – Tamponade is a medical emergency resulting from accumulation of fluid in the pericardium that inhibits heart function. Tamponade is a consequence of the fibrous pericardium being too inelastic to permit adequate heart expansion during diastole. The classic finding is pulsus paradoxus as well as Beck’s triad (low arterial blood pressure, distended neck veins, & soft heart sounds). Treatment is supportive until in a hospital where pericardiocentesis or a pericardial window can be performed to drain the fluid.
- Pericarditis – Inflammation of the pericardium that is typically idiopathic or infectious in nature (the membrane covering the heart). This inflammation is accompanied by swelling at the level of this membrane, in particular due to an excess of fluid circulating between the pericardium and the heart. The main symptoms of pericarditis are pain in the chest. These pains can occur suddenly, sharply and severely. The pain is usually worse at night when lying down and less when sitting. Treatment of viral & idiopathic pericarditis is NSAIDs or aspirin.
Disorders of the heart valves
- Disorders of the heart valves
- Specific valvular problems – Specific problems of each valve.
- Aortic valve – Disorders and treatments of the aortic valve that separates the left ventricle and aorta.
- Aortic regurgitation / aortic insufficiency – Deficiency of the aortic valve that permits regurgitation from the aorta into the left ventricle.
- Aortic stenosis – Narrowing of the aortic valve opening that reduces blood flow through the valve. Stenosis commonly occurs from calcification of the valve, which happens prematurely in those with a bicuspid aortic valve. Stenosis of the aortic valve produces a harsh systolic murmur that classically radiates in the carotid arteries as well as pulsus parvus et tardus.
- Aortic valve replacement – Replacement of the aortic valve due to aortic regurgitation, aortic stenosis, or other reasons. A special kind of replacement called percutaneous aortic valve replacement is done through catheters are does not require open-heart surgery.
- Aortic valve repair – Repair, instead of replacement, of the aortic valve.
- Aortic valvuloplasty – Repair of the valve by using a balloon catheter to force it open.
- Mitral valve – Disorders and treatments of the mitral valve that separates the left atrium and left ventricle.
- Mitral valve prolapse – Prolapse of the mitral valve into the left atrium during ventricular systole.
- Mitral regurgitation / mitral insufficiency – Deficiency of the mitral valve that permits regurgitation from the left ventricle into the left atrium. Regurgitation produces a systolic murmur that radiates into the axilla.
- Mitral stenosis – Narrowing of the mitral valve opening that reduces blood flow through the valve.
- Mitral valve replacement – Replacement of the mitral valve due to mitral regurgitation, mitral stenosis, or other reasons.
- Mitral valve repair – Repair, instead of replacement, of the mitral valve.
- Mitral valvuloplasty – Repair of the valve by using a balloon catheter to force it open.
- Pulmonary valve – Disorders of the pulmonary valve that separates the right ventricle and pulmonary artery.
- Pulmonary regurgitation / pulmonary insufficiency – Deficiency of the pulmonary valve that permits regurgitation from the pulmonary artery into the right ventricle.
- Pulmonic stenosis – Narrowing of the pulmonary valve opening that reduces blood flow through the valve.
- Tricuspid valve – Disorders of the tricuspid valve that separates the right atrium and right ventricle.
- Tricuspid regurgitation / tricuspid insufficiency – Deficiency of the tricuspid valve that permits regurgitation from the right ventricle into the right atrium.
- Tricuspid stenosis – Narrowing of the tricuspid valve opening that reduces blood flow through the valve.
- Ebstein’s anomaly – A congenital heart defect that results in the tricuspid valve leaflets being deeper in the heart (toward the apex) than normal. The annulus of the valve is in the correct position, however, and the portion of the ventricle affected becomes “atrialized” with thinner walls. The right atrium becomes hypertrophied and can result in conduction defects (e.g., Wolff–Parkinson–White syndrome).
- Tricuspid atresia – A congenital heart defect that results in the absence of the tricuspid valve
- Aortic valve – Disorders and treatments of the aortic valve that separates the left ventricle and aorta.
- Endocarditis – The thin, inner lining of the heart is the endocardium and inflammation of this layer is called endocarditis. Endocarditis commonly affects the heart valves.
- Infective endocarditis – Commonly affects the valves due to absence of blood supply to the heart valve, which results in a decreased immune response to the valve leaflets. Typically, bacteria cause infective endocarditis of the mitral valve, but intravenous drug users (e.g., heroin, methamphetamine) have an increased risk of infection of the tricuspid valve. Common signs include Janeway lesions (non-tender), Osler’s nodes (tender), and splinter hemorrhage of the nails.
- Nonbacterial thrombotic endocarditis (NBTE) – Growths on the valves that are not from an infectious source and are composed of fibrin and platelets, and is associated with a history of rheumatic fever. The aortic valve is the most common valve affected (followed by mitral, tricuspid, & then pulmonary).
- Libman–Sacks endocarditis – A form of nonbacterial endocarditis specific to systemic lupus erythematosus (SLE) and tends to affect the mitral valve (unlike NBTE which affects the aortic valve). It is the second most common heart finding in SLE after pericarditis
- Specific valvular problems – Specific problems of each valve.
Congenital heart defects
- Congenital heart defects – defects in the structure of the heart which are present at birth and are often the result of aberrant embryological development. Defects can be syndromic or non-syndromic, with the later meaning defects that are isolated and not found in patterns (i.e., a syndrome). The top two syndromic causes of congenital heart defects are Noonan syndrome and Down syndrome. Down syndrome is more common than Noonan syndrome, but has a lower incidence of congenital heart defects, which makes Noonan syndrome the most common syndromic cause of congenital heart defects.
- Atrial septal defect (ASD) – Defect in the interatrial septum that permits blood flow between atria, including a patent foramen ovale (PFO).
- Bicuspid aortic valve – Formation of two valve leaflets in the aortic valve instead of three leaflets. This leads to aortic stenosis as the valve prematurely calcifies (as compared to calcification of a trileflet valve).
- Coarctation of the aorta (CoA) – Narrowing of the aorta, typically of the aortic arch and is classically found in Turner syndrome. A “complete” coarction is called an interrupted aortic arch.
- Cor triatriatum – A membrane that divides one of the atria results in “three” atria (hence “triatriatum“). This tends to affect the left atrium more than the right atrium. The membrane may be present without complete division of the atrium. It presents similarly to stenosis of the respective semilunar valve (i.e., tricuspid stenosis for right atrium).
- Dextrocardia – Dextrocardia is a condition in which the apex of the heart is on the right side of the body, instead of the left. This can exist in isolation or as a part of situs inversus in which the entire body is mirrored not just the heart. Situs inversus can be a part of primary ciliary dyskinesia (aka Kartagener syndrome) that has recurrent respiratory infections and male infertility. A simple chest xray is sufficient to diagnose dextrocardia, provided care is taken in marking the correct side of the radiograph.
- Ebstein’s anomaly – Malformation of the tricuspid valve (see above).
- Great artery defects – There are several conditions that affect the great arteries (e.g., double aortic arch, aberrant subclavian artery) that often result in problems with the trachea and breathing.
- Hypoplastic left heart syndrome – Defect in the development of the left heart such that it is hypoplastic (under developed).
- Patent ductus arteriosus (PDA) – Failure of the ductus arteriosus to close on birth.
- Patent foramen ovale (PFO) – An atrial septal defect in that the foramen ovale fails to close at birth.
- Persistent truncus arteriosus – Defect in that the truncus arteriosus fails to divide.
- Pulmonary valve stenosis (PVS) – Narrowing of the pulmonary valve that is the key finding in Noonan syndrome.
- Tetralogy of Fallot (ToF) – Set of four anatomical abnormalities: pulmonary stenosis, overriding aorta, ventricular septal defect, and right ventricular hypertrophy.
- Transposition of the great vessels (TGV) – Abnormal spatial arrangement of the great vessels (superior vena cava, inferior vena cava, pulmonary arteries, pulmonary veins, and aorta).
- Uhl anomaly – Partial or total loss of the right ventricular wall.
- Ventricular septal defect (VSD) – Defect in the ventricular septum that permits blood flow between ventricles.
Diseases of blood vessels
- Diseases of blood vessels – diseases of the blood vessels can be multidisciplinary in nature. For example, medical treatment of atherosclerosis tends to be managed by cardiologists while vascular surgery repairs aneurysms and stenotic arteries.
- Atherosclerosis – Thickening of an arterial wall due to increased cholesterol and macrophages (see above).
- Aneurysm – Balloon-like bulging of arteries (also possible of the heart: see ventricular aneurysm above).
- Aortic aneurysm – Aneurysm of the aorta, typically of the abdominal aorta (abdominal aortic aneurysm or AAA). They are associated with a smoking history and in connective tissue diseases (e.g., Marfan syndrome, Ehlers-Danlos syndrome). Current USPSTF recommendations are for a single abdominal ultrasound screening for a AAA in anyone 65 or older who has smoked. Surgical repair of a AAA is advised after it is larger than 5.0–5.5 cm because of concern for rupture that leads to death from internal bleeding.
- Cerebral aneurysm – Aneurysms of the arteries in the brain most commonly affect the anterior cerebral artery. Rupture of the aneurysm results in a subarachnoid hemorrhage and a very severe headache.
- Aortic dissection – Dissection along the length of the aorta between the layers of the aortic wall. Dissection of the ascending aorta (type A) is a surgical emergency while dissection of the descending aorta (type B) can possibly be managed medically. Dissection of the ascending aorta is an emergency because dissection may interrupt coronary blood flow and blood flow to the brain, neither of which tolerate ischemia particularly well.
- Aortic rupture – Frank rupture of the aorta is often fatal from internal bleeding. Rupture of the aorta can occur at the sites of aneurysm, but is also due to trauma and results in a traumatic aortic rupture.
- Carotid artery – Diseases of the carotid arteries:
- Carotid artery stenosis / carotid artery disease – Narrowing of the carotid artery, typically due to atherosclerosis.
- Carotid artery dissection – Dissection along the length of the carotid artery between the layers of the carotid wall and filled with blood.
- Deep vein thrombosis (DVT) and pulmonary embolism (PE) – Formation of a thrombus in a deep vein, commonly in the legs that may break loose, travel to the lungs, and occlude blood flow (pulmonary embolism) sufficient to interrupt oxygenation to the body.
- Traveller’s thrombosis / economy class syndrome: A DVT due to being sedentary during air travel.
- Microangiopathy – Disease of capillaries in which the walls become thick and weak, and result in bleeding and decreased blood flow. One very common cause is diabetes mellitus in which microangiopathy results in diabetic nephropathy, diabetic retinopathy, and diabetic neuropathy.
- Varicose veins – Veins that have become enlarged and tortuous with failed valves, commonly in the legs. Vericose veins have cosmetic concerns, but they may become painful. Surgery and sclerotherapy are two options for treating varicose veins.
- Vasculitis – Inflammation of blood vessels (veins & arteries) with a long list of causes.
- Aortitis – Inflammation of the aorta that can be seen in giant cell arteritis, polymyalgia rheumatica, rheumatoid arthritis, syphilis and Takayasu’s arteritis.
- Behçet’s disease – Affects small-sized vessels that often initially presents with oral aphthous ulcers, genital ulcers and uveitis, and can be fatal from ruptured aneurysms. Pericarditis is commonly seen with Behçet’s.
- Eosinophilic granulomatosis with polyangiitis (EGPA; formerly known as Churg-Strauss syndrome) – Affects small- & medium-sized vessels that often affects lungs, kidneys, & heart in those with a history of airway allergic hypersensitivity and p-ANCA antibodies.
- Giant-cell arteritis (GCA) / Temporal arteritis – Affects medium- & large-sized vessels of the head, typically branches of the external carotid artery and namely the temporal artery. Occlusion of the ophthalmic artery results in blindness. Suspicion of GCA necessitates immediate treatment with glucocorticoids and temporal artery biopsy.
- Granulomatosis with polyangiitis (GPA) – Affects small- & medium-sized vessels that often affects the lung & kidneys (RPGN) with classic saddle nose and c-ANCA antibodies.
- IgA vasculitis (IgAV; formerly known as Henoch-Schönlein purpura) – Affects small-sized vessels and produces palpable purpura and proteinuria from immunocomplex (IgA) deposition.
- Kawasaki disease – Affects medium-sized vessels mostly seen in young children with myocarditis, & pericarditis, and is the most common cause of acquired heart disease in children (results in coronary artery aneurysms). Myocardial infarction from coronary thrombosis is the most common cause of death from Kawasaki disease.
- Thromboangiitis obliterans – Affects small- & medium-sized vessels that is strongly associated with tobacco products. Pain, diminished pulses, gangrene and eventual amputation of affected hands and feet.
Risk and prevention heart diseases
Prevention is essential!
Cardiovascular disease is one of the leading deaths among many countries. Therefore it is important to understand how to prevent them.
Lifestyle risk factors
Small, healthy changes in your daily routine can lower your risk of heart disease.
Risk factors you can’t control:
Sex
Your risk of heart disease and stroke increases after menopause… In fact, most women across the country have at least one risk factor associated with heart disease and stroke. Women who have diabetes, those from certain ethnic groups, and those going through the menopause are at even greater risk.
Age
The risk of heart diseases increases with age.
Family and medical history
Your risk is higher if one of your close relatives has had heart disease at a young age.
Personal situation
Your personal situation and environmental factors influence your health. These are conditions like accessibility to healthy food, clean water, health care and social services.
Preventing heart diseases
Set a goal that will inspire you to be healthier. These are some examples:
Eat healthy
Eating a healthy diet, that is, eating a balanced diet, is one of the most effective ways to protect your health. Vegetables and fruits contain a lot of nutrients. Aim for 7 to 10 servings each day.
Your diet can help reduce your risk of heart disease and stroke by:
- improving your cholesterol level;
- lowering your blood pressure;
- helping you manage your weight;
- controlling your blood sugar levels.
Prevention of heart disease by eating healthy
Many vegetables and fruits are particularly rich in vitamin C and beta-carotene, a form of vitamin A. These substances act as antioxidants in your body and help slow or prevent atherosclerosis by reducing the build-up of plaque formed by cholesterol and other substances inside the arteries. The great champions of vitamin C are:
- broccoli;
- red pepper;
- the strawberry;
- oranges;
- kiwis;
- cantaloupe.
Beta-carotene gives foods a distinctive red, orange or dark green color, so it’s easy to identify the best sources, such as:
- the carrot;
- tomatoes;
- squash;
- pink grapefruit;
- sweet potato;
- Swiss chard.
Plus, almost all vegetables and fruits are low in calories, fat, and sodium. In fact, research shows that eating high vegetables and fruit is associated with maintaining a healthy weight.
A good source of fiber
Eating vegetables and fruits is an excellent source of fiber. When possible, eat the peel as well, as it increases your daily fiber intake. For example, a raw apple with its peel contains 10 times more fiber than 250 ml (1 cup) of apple juice.
Fresh and frozen products
Frozen or canned vegetables and fruits have about the same nutritional value as fresh ones. When buying canned or frozen fruit, look for products without syrup or added sugar. So fruit canned in water is the best option.
In order to retain as many nutrients as possible, the best cooking methods are steaming, roasting, or broiling. If you are using canned vegetables, look for varieties with no added salt or rinse them under running water to remove most of the added salt.
Protein can be obtained from several different sources, including:
- legumes;
- nuts;
- seeds;
- tofu;
- fortified soy beverages;
- Fish;
- seafood;
- eggs;
- Poultry;
- lean red meats, including game;
- low fat milk;
- low fat yogurts;
- low-fat kefir;
- cheeses low in fat and salt;
- some grains.
When choosing your protein sources, it’s important to aim for variety. Aim to have at least two servings of fish each week and consume beans, lentils, and tofu on a regular basis. When buying meat, take it lean and go for servings of around 110 g (4 oz), which is the size of your palm.
Keep fit
To maintain a healthy heart, a little physical activity is very beneficial. Here are some tips for moving.
Exercise is the closest approach to the fountain of youth for anyone seeking eternal youth. Regular physical activity can help you reach and maintain a healthy weight, stay in shape, slow down the physical decline that accompanies aging, sleep better, reduce stress levels… and much more!
Try to be physically active every day. Walk to work, take a lunch break from being physically active, or take a walk after dinner. If you make activity part of your routine, you’ll find that it becomes easy and fun, and you don’t feel like you’re wasting time doing it.
Choose activities that you enjoy. This way, it’s more likely that you won’t give up. If you hate gyms, walk the hiking trails, garden, golf, or sign up for yoga classes.
Reduce stress
Managing stress will help you feel better every day and lower your risk for cardiovascular disease.
Stress can increase your risk for heart disease and stroke, and lead to depression or anxiety. It is therefore important that you are able to recognize and deal with your stress.
Healthy weight
Adopt healthy habits and a healthy weight – for life.
Controlling your weight doesn’t necessarily mean changing your lifestyle at all. Take it in small steps, set small, realistic goals for yourself, and then build from there. A small steady weight loss of 1 or 2 pound (½ to 1 kg) per week is easier to achieve and healthier for your heart than a large and sudden loss. Studies also show that you will be less likely to regain that lost weight.
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, World Health Organization, Web MD, NHS UK, American Heart Association, Pan American Health Organization, Mayo Clinic
Photo credit (main picture): Wellcome Collection (Public Domain Mark 1.0)