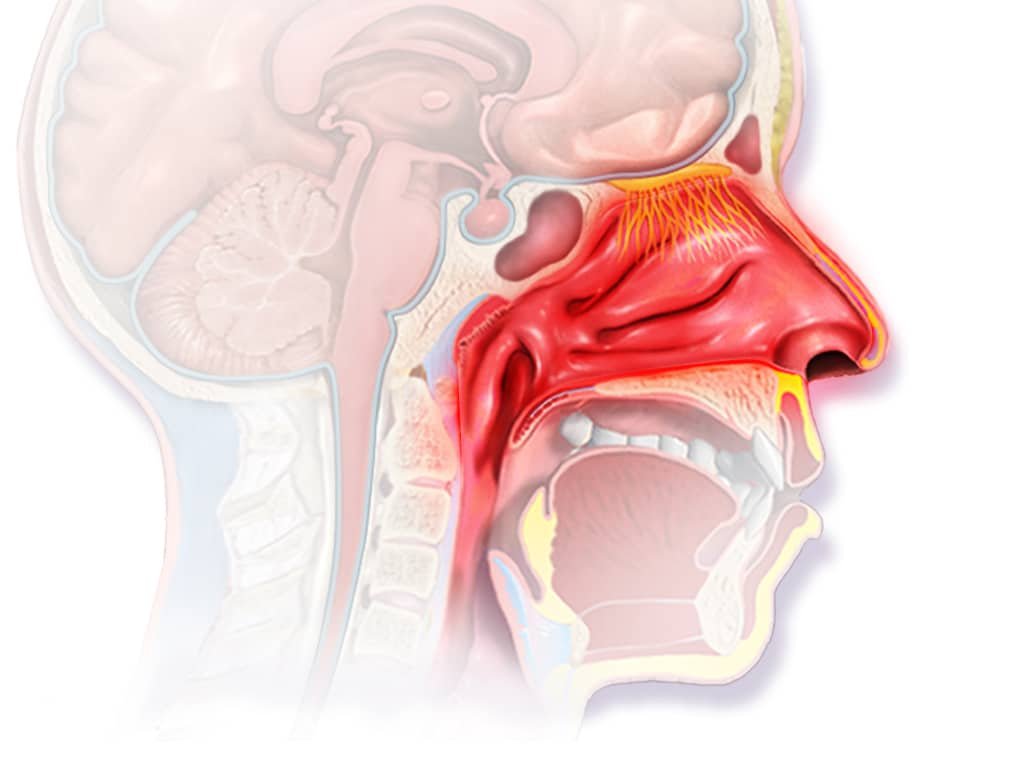
Rhinitis
Rhinitis is inflammation of the nasal mucosa (part of the respiratory), resulting in nasal congestion, rhinorrhea, and associated symptoms that vary by cause or origin specifically (eg, pruritus, sneezing, purulent or clear rhinorrhea, anosmia). Rhinitis is classified as allergic or non-allergic. The cause of nonallergic rhinitis is usually viral, although irritants may be involved. The diagnosis is usually clinical. The treatment can combine the humidification of the ambient air, vasoconstrictors (sympathomimetic amines) and antihistamines. Bacterial superinfection requires adequate antibiotic treatment.
Nonallergic rhinitis
There are several forms of non-allergic rhinitis. For allergic rhinitis, see Allergic Rhinitis | Symptoms, causes, treatments and prevention
Acute rhinitis
Acute rhinitis, manifested by edema and vasodilation of the nasal mucosa, rhinorrhea and occlusion, are usually the result of a common cold; other causes include streptococcal, pneumococcal, and staph infections.
Chronic rhinitis
Generally corresponds to an extension (resolved within 30 to 90 days) of subacute inflammatory or infectious rhinitis. It may also rarely be related to syphilis, tuberculosis, rhinosclerosis, rhinosporidiosis, leishmaniasis, blastomycosis, histoplasmosis, and leprosy, all of which are infections characterized by granuloma formation and soft tissue destruction. , cartilage and bone. Nasal obstruction, purulent rhinorrhea and frequent bleeding result. Rhinosclerosis also induces progressive nasal obstruction due to the presence of indurated inflammatory tissue in the lamina propria. Rhinosporidiosis is characterized by bleeding polyps. Low humidity and airborne irritants can cause chronic rhinitis.
Atrophic rhinitis
Is a form of chronic rhinitis, induces mucosal atrophy and sclerosis; the ciliated pseudostratified columnar epithelium of the mucosa transforms into squamous epithelium and the thickness and vascularity of the lamina propria decreases. Atrophic rhinitis is associated with advanced age, granulomatosis with polyangiitis (formerly called Wegener’s granulomatosis), and excessive excision of the nasal mucosa. Although the exact cause or origin specifically is unknown, bacterial infection is a likely co-factor. Atrophy of the nasal mucosa is often observed in elderly patients.
Vasomotor rhinitis
Also called nonallergic rhinitis, is a chronic disease in which intermittent vascular engorgement of the nasal mucosa causes clear rhinorrhea and sneezing. The cause or origin specifically is uncertain, and no allergy is identifiable. A dry atmosphere seems to aggravate this situation.
Symptoms of non-allergic rhinitis
Acute rhinitis induces cough, moderate fever, nasal congestion, rhinorrhea and sneezing.
Manifestations of chronic rhinitis are similar to those of acute rhinitis, but in prolonged or severe cases, patients may also have thick, foul-smelling, mucopurulent drainage; mucous crusts; and/or bleeding.
Atrophic rhinitis causes enlargement of the nasal cavities, crusting and malodorous bacterial colonization, nasal congestion, anosmia and epistaxis which may be recurrent and severe.
Vasomotor rhinitis induces sneezing and watery rhinorrhea. The turgid mucosa varies from bright red to purple. The disease is characterized by periods of remission or worsening.
Diagnosis of non-allergic rhinitis
The different forms of rhinitis are diagnosed clinically. Complementary examinations are unnecessary.
Vasomotor rhinitis is differentiated from specific viral and bacterial infections of the nose by the absence of discharge and purulent crusts. It is distinguished from allergic rhinitis by the absence of an identifiable allergen.
Treatment of non-allergic rhinitis
- In viral rhinitis, decongestants and/or antihistamines
- For atrophic rhinitis, topical treatment with antibiotics, estrogen, and vitamins A and D
- In vasomotor rhinitis, humidification and sometimes topical corticosteroids and oral pseudoephedrine
Viral rhinitis can be treated symptomatically with decongestants (either local vasoconstriction with a sympathomimetic amine, such as oxymetazoline every 8-12 hours or phenylephrine 0.25% every 3-4 hours for no more than 7 days or systemic sympathomimetic amines, such as pseudoephedrine 30 mg orally every 4 to 6 hours). Antihistamines (see table Inhaled Nasal Mast Cell Stabilizers) may help, but those with anticholinergic properties dry the mucous membranes and may increase irritation. (See also Common Cold.) Decongestants can also relieve symptoms of acute bacterial rhinitis and chronic rhinitis, where an underlying bacterial infection requires swabs for pathogen identification, susceptibility testing, and appropriate antimicrobial treatment. If symptoms persist, a biopsy may be needed to rule out cancer.
Treatment of atrophic rhinitis aims to reduce scabs and eliminate odor through nasal irrigation using antibiotics (eg, bacitracin, mupirocin), local or systemic estrogen, and vitamins A and D. Occlusion of the nasal cavities or reduction of their patency by surgery decreases the formation of crusts due to the drying effect of the air circulating on the atrophic mucosa.
The treatment of vasomotor rhinitis is empirical on a case-by-case basis and is not always satisfactory. Patients are improved by air humidification, such as a humidified central heating system or a humidifier placed in the office or bedroom.
Topical corticosteroids (eg, mometasone 2 sprays twice a day) and nasal antihistamines may help. Systemic sympathomimetic amines (eg, in adults, pseudoephedrine, 30 mg orally every 4 to 6 hours as needed) decrease symptoms but are not recommended for prolonged use because they thicken the mucus and can cause tachycardia and nervousness.
Local vasoconstrictors should be avoided because the nasal mucosa vasculature loses its sensitivity to other vasoconstrictor stimuli, e.g. eg, the humidity and temperature of the inspired air. Rebound may occur after 3-5 days of continuous use; chronic use and addiction is called rhinitis medicamentosa.
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, The Johns Hopkins University, Mayo Clinic, NHS UK
Photo credit: Blausen Medical / Wikimedia Commons (CC BY 3.0)
Author: Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014“. Wiki Journal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.