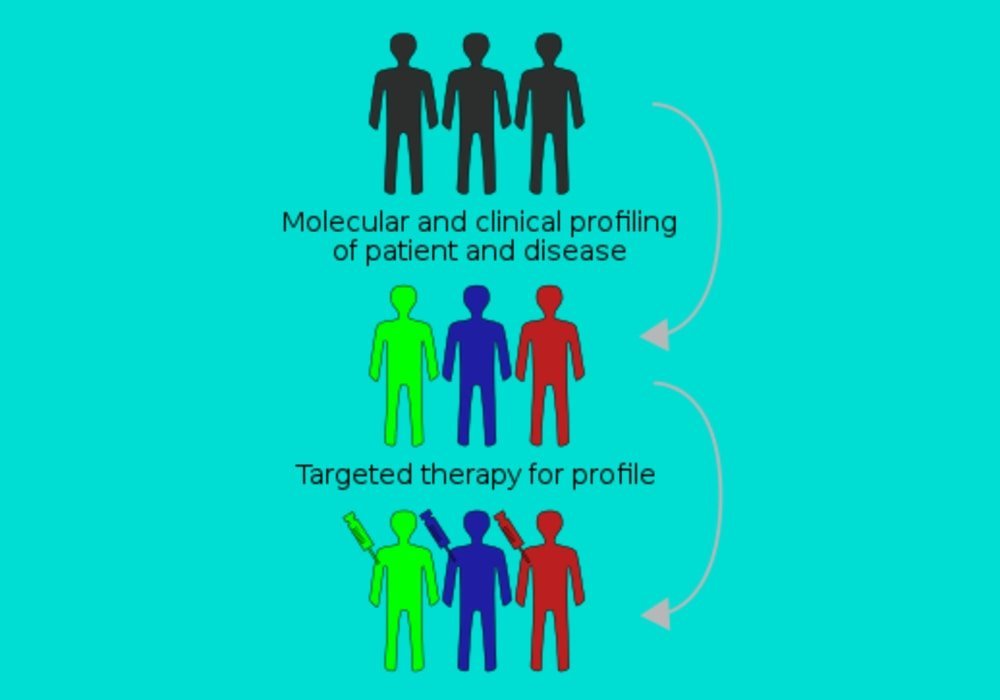
Targeted therapy for cancer patients
Targeted therapy uses drugs to target specific molecules, such as proteins, on the surface or inside of cancer cells. Targeted therapy is also called molecular targeting therapy. It is administered for:
- slow the growth of cancer;
- destroy cancer cells;
- relieve symptoms caused by cancer.
There are different types of targeted drugs. Each one acts differently depending on the molecule (gene or protein) targeted by the drug. The treatment is chosen according to the types of molecules produced by the tumor. Some targeted drugs target specific proteins in cancer cells that are not found in normal cells. Other targeted drugs target mutated proteins or mutated genes in cancer cells. This allows doctors to tailor cancer treatment to each person. Targeted therapy is an important part of personalized, or precision medicine, which uses information about a person’s genes and proteins to prevent, diagnose and treat cancer.
How targeted therapy works?
Targeted therapy targets molecules that send signals to cancer cells telling them to grow or divide. By targeting these molecules, the drugs block their signals and stop the growth and spread of cancer cells while harming normal cells as little as possible.
Targeted therapy is only effective if a cancer cell carries the genetic or protein target that the medicine is trying to block. This is why it is not given to every person with cancer. Those who receive targeted therapy should first have specific tests to know if their tumor has these targets. But even if a certain target is in a person, it does not mean that the targeted therapy will be effective. This may be because the protein or gene targeted by the treatment is only partly responsible for the growth of the tumor. Targeted therapy often does not cure cancer on its own, but it can be very helpful when combined with other types of cancer treatment such as surgery, chemotherapy and radiation therapy.
Types of targeted therapy
Most targeted treatments are monoclonal antibodies or small molecule drugs. Monoclonal antibodies bind to proteins or genes on the surface of cells. They are large and do not easily enter cells. Small molecule drugs are among many other types of target drugs that are not monoclonal antibodies. These drugs are made up of molecules that are smaller than antibodies. Small molecule drugs easily enter cells. They bind to proteins inside cells and block their actions. Tyrosine kinase inhibitors as well as proteasome inhibitors are examples of small molecule drugs.
Targeted drugs are also grouped by the protein they target or how they work. Some targeted drugs belong to more than one group.
1. Monoclonal antibodies
Monoclonal antibodies are variants of proteins in the immune system called antibodies that are designed in the laboratory. Monoclonal antibodies block a target on the outer surface of the cancer cell. The target is often another type of protein. They do this by recognizing the protein and attaching itself to it, preventing it from doing its job. Monoclonal antibodies can also help chemotherapy drugs and radiation enter and destroy cancer cells. They do this by attaching to a protein on the cell’s surface to allow chemotherapy drugs or radiation to be absorbed by the cancer cell. Monoclonal antibodies are usually given by injection into a vein (intravenously).
Some types of monoclonal antibodies are also used as immunotherapy, because they trigger the immune system to attack and destroy cancer cells. Monoclonal antibodies are easy to recognize since their name always ends with “mab”. The following monoclonal antibodies are often used to treat cancer.
Trastuzumab (Herceptin)
It targets tumors that contain a lot of HER2 protein, known as HER2 positive tumors. Too much HER2 protein is produced when there is a mutation in the ErbB2 (HER2) gene, causing it to make too many copies of itself. Trastuzumab is used to treat HER2 positive cancers, including cancers of the breast, stomach and esophagus.
Bevacizumab (Avastin)
It binds to vascular endothelial growth factor receptor (VEGF) proteins found on cancer cells. It is used to treat cancers that make a lot of VEGF receptor proteins, including cervical and ovarian cancers and colorectal cancer.
Rituximab (Rituxan)
It binds to the CD20 protein found on B cells. It is most often used to treat types of non-Hodgkin lymphoma with high abnormal B cell counts.
Cetuximab (Erbitux)
It binds to epidermal growth factor receptor (R-EGF) proteins found on cancer cells. It is used to treat cancers that make a lot of R-EGF protein, including colorectal cancer and certain types of head and neck cancer.
2. Tyrosine kinase inhibitors
Tyrosine kinase is a component of protein that acts as a cell’s on-off switch. It is an enzyme that plays an important role in the growth and division of cells. Tyrosine kinase inhibitors prevent these enzymes from sending signals that tell the cancer cell to grow. These drugs are also called signal transduction inhibitors.
The following are examples of tyrosine kinase inhibitors.
Imatinib (Gleevec) targets tyrosine kinase which causes cancer to grow out of control. Imatinib is most often used to treat certain types of leukemia that carry the Philadelphia chromosome.
Gefitinib (Iressa) works on cancer cells that carry the epidermal growth factor receptor (R-EGF) protein. It targets the protein tyrosine kinase. It is sometimes used to treat non-small cell lung cancer, but it has also been tested for effectiveness in other types of cancer that have high R-EGF proteins.
3. Apoptosis inducers
The natural process of cell death is a series of programmed events called apoptosis. In some cancer cells, the signals that tell them to begin to self-destruct are incorrect. Apoptosis inducers help restore these signals that tell cancer cells to die. These drugs interfere with certain proteins, or enzymes, that help cells grow and survive. Apoptosis inducers can also make it easier to destroy cancer cells with chemotherapy.
Here are some examples of apoptosis inducers.
Bortezomib (Velcade) is a proteasome inhibitor. It blocks a group of proteins (proteasomes) necessary for the development of cancer cells. Impeding the function of proteasomes can help cancer cells to die.
Oblimersen (Genasense) is an antisense medicine. It blocks the production of a protein known as Bcl-2, which helps cancer cells survive and can cause resistance to cancer drugs. Blocking the activity of Bcl-2 can make cancer cells more sensitive to cancer drugs.
Olaparib (Lynparza) is a poly (ADP-ribose) polymerase (PARP) inhibitor. PARPs are enzymes that help repair DNA damage. PARP inhibitors block PARPs so that cancer cells are unable to repair their DNA, which causes their death.
4. Angiogenesis inhibitors
Angiogenesis is the formation of new blood vessels. A tumor has to make new blood vessels to grow, so antiangiogenic drugs try to cut off the tumor’s blood supply by preventing it from forming new blood vessels. Here are some examples of angiogenesis inhibitors.
Bevacizumab (Avastin) binds to vascular endothelial growth factor receptor (VEGF) proteins found on cancer cells. It blocks VEGF and helps treat cancers that produce lots of VEGF receptor proteins. Bevacizumab is also a type of monoclonal antibody.
Sunitinib (Sutent) blocks VEGF which causes blood vessels to form. It also binds to VEGF receptor proteins found on cancer cells. Sunitinib is also a type of tyrosine kinase inhibitor that prevents the growth of cancer cells.
Thalidomide (Thalomid) interferes with the signals inside cancer cells that cause new blood vessels to form. It is most often used to treat multiple myeloma.
5. MTOR inhibitors
MTOR inhibitors block the mammalian target of rapamycin (mTOR). MTOR is a protein that controls the growth and division of cells. In some types of cancer, mTOR does not work properly, causing cancer cells to grow and divide uncontrollably. MTOR inhibitors block the action of mTOR, which can stop the growth of some types of cancer. MTOR inhibitors are used to treat kidney cancer and some neuroendocrine tumors. Examples are temsirolimus (Torisel) and everolimus (Afinitor).
6. Hormone therapy
Hormonal drugs are a type of targeted drug. They block hormones like estrogen, progesterone and testosterone from binding to receptors that help cancer cells to grow.
Find out more about hormone therapy.
Hormone Therapy: What It Is, How It Works, and Its Use in Medical Treatment
7. Tumoricidal bacteria
Therapeutic strategies based on tumoricidal bacteria (or carcinolytic bacteria) are targeted therapies that have been known for a long time for some, and still experimental for the most part. When bacteria of this type are administered into the body, they migrate to cancerous tissues and begin to grow, then deploy their respective mechanisms to destroy solid tumors. Each species of bacteria uses a different process to eliminate the tumour.
Common tumoricidal bacteria include Salmonella, Clostridium, Bifidobacterium, Listeria, and Streptococcus. The first research on this type of bacteria was highlighted in 1813 when scientists observed that patients with gas gangrene, an infection caused by Clostridium bacteria, could cause tumor regressions.
A genetically engineered strain of Salmonella (TAPET-CD) has completed Phase 1 clinical trials for patients with stage 4 metastatic cancer. Cancer vaccines based on Listeria are currently being produced and undergoing numerous trials clinics. Phase I trials of the Clostridium strain called Clostridium novyi (C. novyi-NT) for patients with treatment-refractory tumors or tumors that do not respond to treatment are currently underway.
Receiving targeted treatment and the process
Targeted therapy can be given in different ways: as pills or capsules that you swallow (orally) or through a needle inserted into a vein (intravenously).
Some targeted drugs can only be given in a hospital. Others can be taken at home. Targeted therapy takes place according to a set schedule, or protocol, which is determined by your condition. Each session usually consists of a treatment period followed by a recovery period.
Sometimes, only targeted therapy is given, but it is often used in combination with other types of therapy such as chemotherapy, radiation therapy, or both.
Side effects of targeted therapy
Regardless of the treatment, side effects may occur. Side effects of targeted therapy tend to be mild and go away once the body gets used to the medicine. Targeted therapy attacks cancer cells and limits damage to healthy cells, so side effects are usually fewer and less severe than with chemotherapy and radiation therapy. If some side effects are serious, your doctor may stop treatment for a while or adjust the dose. The side effects of targeted therapy mainly depend on the following:
- the type of drug, drug combination or combination of treatments
- the dose
- the method of administration (by mouth or into a vein for example)
- your overall health
Side effects of targeted therapy may include the following:
Skin problems
Some types of targeted drugs may cause skin problems during treatment and for some time afterward. The skin may become red, itchy, dry, and start to peel or crack. You may also have a rash or acne. The area around the injection site may swell or redden. Shortly after the injection, a rash sometimes occurs around the injection site.
The nails may also undergo changes as a result of the targeted therapy. The skin around the nails may swell and redden, and cracks or open lesions may appear.
When radiation therapy is given at the same time as targeted therapy, skin problems tend to be more serious.
Your healthcare team may offer lotions, creams, or other medicines to relieve skin problems. It is important to protect your skin from the sun during targeted therapy, as sun exposure can make skin problems worse.
Increased blood pressure
Some targeted drugs can cause high blood pressure (hypertension). Blood pressure is regularly assessed during treatment. Sometimes the dose of the drug may be changed to treat blood pressure problems or a drug to lower blood pressure is given while continuing targeted therapy.
Bleeding or blood clots
Angiogenesis inhibitors can cause bleeding in the stomach or intestine. Signs of bleeding include vomiting blood or something that looks like coffee grounds. You may also have blood in your stool.
Angiogenesis inhibitors can also cause blood clots. This is a rare but serious side effect. The formation of a blood clot in one leg is called deep vein thrombosis (DVT). In more severe cases, the blood clot may break off and travel to the lungs (pulmonary embolism, or PE). This can cause shortness of breath, bloody coughing, low blood oxygen levels, or heart failure in some cases.
Low doses of medicines that thin the blood may be given to help reduce the risk of blood clots. Tell your healthcare team right away if you have redness, swelling, pain or cramps in your calf, shortness of breath, bloody cough, or blood in your stool.
Poor wound healing
Targeted drugs can slow wound healing and increase the risk of other wound complications, such as infection. Targeted drugs related to poor wound healing, such as angiogenesis inhibitors, are often stopped before scheduled surgery.
Long term side effects of cancer treatment (Late effects) for cancer survivors
Report side effects
Be sure to mention your side effects to the healthcare team. Your team is there for you. Side effects can occur anytime during, immediately after, or a few days or even a few weeks after targeted therapy. Sometimes side effects may appear months or years after targeted therapy. Most go away on their own or can be treated, but some may last a long time or be permanent.
List of all Cancers
The word “cancer” is a generic term for a large group of diseases that can affect any part of the body. We also speak of malignant tumors or neoplasms. One of the hallmarks of cancer is the rapid multiplication of abnormal growing cells, which can invade nearby parts of the body and then migrate to other organs. This is called metastasis, which is the main cause of death from cancer. Types of cancer (in alphabetical order of the area concerned):
Information: Cleverly Smart is not a substitute for a doctor. Always consult a doctor to treat your health condition.
Sources: PinterPandai, The University of Texas MD Anderson Cancer Center, National Cancer Instituteat the National Institutes of Health, American Society of Clinical Oncology (ASCO), National Library of Medicine, Imperial College Healthcare NHS Trust, Verena Staedtke, Nicholas J. Roberts, Ren-Yuan Bai et Shibin Zhou, « Clostridium novyi-NT in cancer therapy », Genes & Diseases, vol. 3, no 2, , p. 144–152 (ISSN 2352-4820, PMID 30258882, PMCID 6150096, DOI 10.1016/j.gendis.2016.01.003, résumé [archive]).
Photo credit: Simon Caulton / Wikimedia Commons (CC BY-SA 4.0)